Stroke I Definition I Symptoms I Diagnosis I World Stroke Day 29 oct
World Stroke Day
When someone has a stroke, every second is crucial. The longer it takes to receive treatment, the more likely it is that damage to the brain will occur.
“The mantra is ‘time is brain’. “The sooner they get treatment, the better patients do.”
World Stroke Day is recognized each year on Oct. 29. The aim is to teach the public about stroke risk factors and stroke prevention, and to raise awareness about the warning signs of stroke so people recognize when a loved one may be having a stroke and can take action.
What is Stroke?
A stroke occurs when a blood vessel bringing blood and oxygen to the brain is interrupted or ruptures (bursts) and brain cells don’t get the flow of blood that they need. Deprived of oxygen, nerve cells can’t function and die within minutes. When nerve cells do not function, the part of the body they control can’t function either. The devastating effects of stroke are often permanent because dead brain cells can’t be replaced.
Types of Stroke
There are two main types of strokes: ischemic and hemorrhagic. An ischemic stroke happens when there is a loss of blood supply to an area of the brain. A hemorrhagic stroke happens when there is bleeding into the brain when a blood vessel ruptures. Eighty-five percent of all strokes are ischemic.
Blood supply to the brain
Blood vessels that carry blood to the brain from the heart are called arteries. The brain needs a constant supply of blood, which carries the oxygen and nutrients it needs to function. Each artery supplies blood to specific areas of the brain. A stroke occurs when one of these arteries to the brain either is blocked or bursts. As a result, part of the brain does not get the blood it needs, so it starts to die.
Possible Effects of Stroke
Motor and sensory function
The human brain is divided into several areas that control movement and sensory function, or how the body moves and feels. When a stroke damages a certain part of the brain that area may no longer work as well as it did before the stroke. This can cause problems with walking, speaking, seeing or feeling.
Functions of right and left hemisphere of the brain
The left side, or hemisphere, of the brain controls how the opposite (right side) of the body moves and feels, and is responsible for how well we can figure out problems with science, understanding what we read and what we hear people say, number skills such as adding and subtracting, and reasoning. The right side of the brain controls the movements and feelings on the left side of the body and is in charge of how artistic we are, including musical and creative talents.
Stages of normal and blocked artery blood flow
- Normal artery: Blood flows easily through a clear artery.
- Blockage: An artery can become blocked by plaque (a fatty substance that clogs the artery) or a blood clot, which reduces blood flow to the brain and may cause a stroke.
- Blockage cleared: The plaque or blood clot breaks up quickly and blood flow is restored to the brain. This may happen during a TIA or mini-stroke, where brain cells recover with no permanent brain damage.
Stroke Symptoms from “Fast to Faster” – देखना, दिखना, हाथ, पैर, बोल, चाल
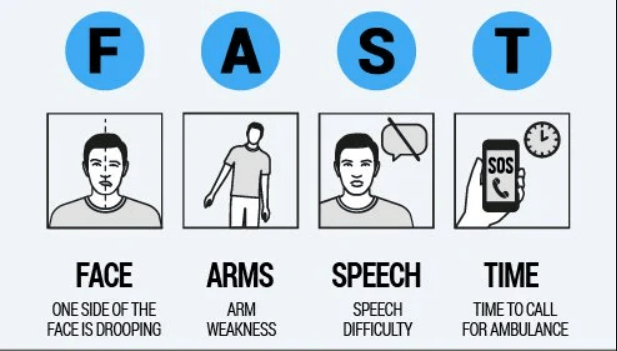
The acronym FAST (Facial drooping, Arm weakness, Speech difficulties and Time) has been used by the National Stroke Association, American Heart Association and others to educate the public on detecting symptoms of a stroke. FAST was first introduced in the United Kingdom in 1998.
Hindi version of FAST is “Dekhna, dikhna, hath, paer, bol, chal” – could be an easy mnemonic. Any sudden onset disturbance in dekhna, dikhna, hath, paer, bol or chal should raise suspicion of a cerebrovascular event and may indicate prompt medical consultation.
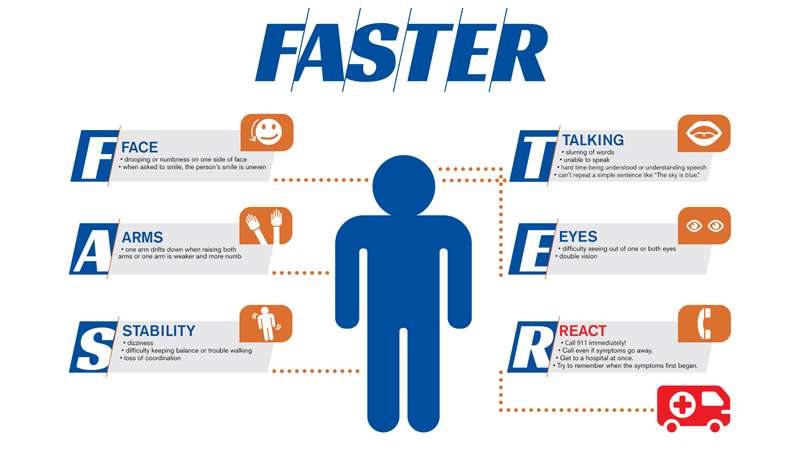
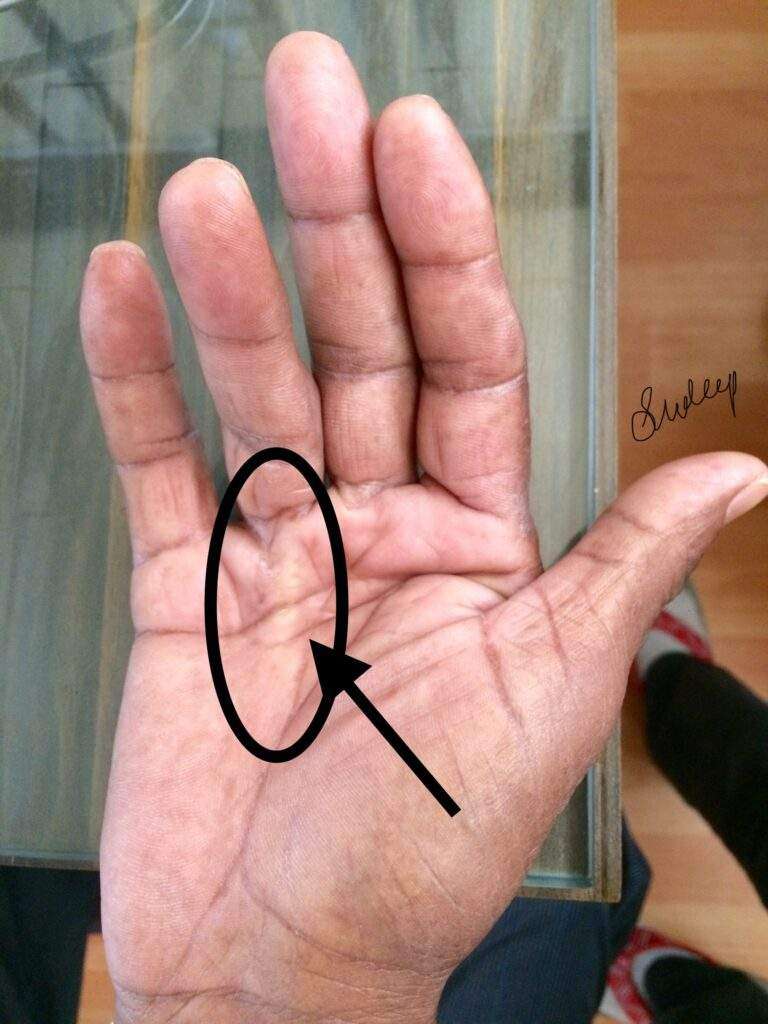
- F stands for Face, which refers to drooping or numbness on one side of the face versus the other. Ask the person to smile to make the droop more apparent.
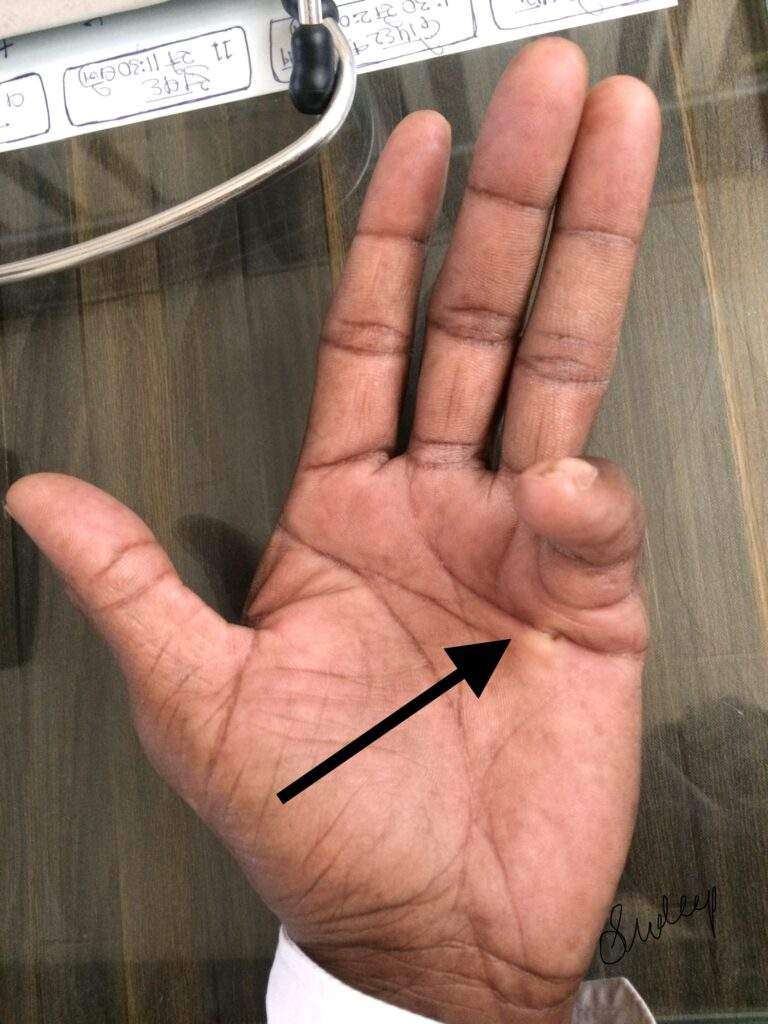
- A stands for Arms, which refers to one arm being weaker or more numb than the other. Ask the individual to raise both arms up and hold them for a count of ten. If one arm falls or begins to drop, then this could be a sign of a stroke.
- S stands for Stability, which refers to steadiness on your feet. Sometimes individuals will fall, feel very dizzy or be unable to stand without assistance. Difficulty maintaining balance, trouble walking and loss of coordination are all possible stroke symptoms.
- T stands for Talking, which refers to changes in speech including slurring, garbled, nonsensical words, or the inability to respond appropriately. Individuals experiencing a stroke may be difficult to understand, or they may have difficulty understanding others. Ask the person to repeat a simple sentence like “The sky is blue.”
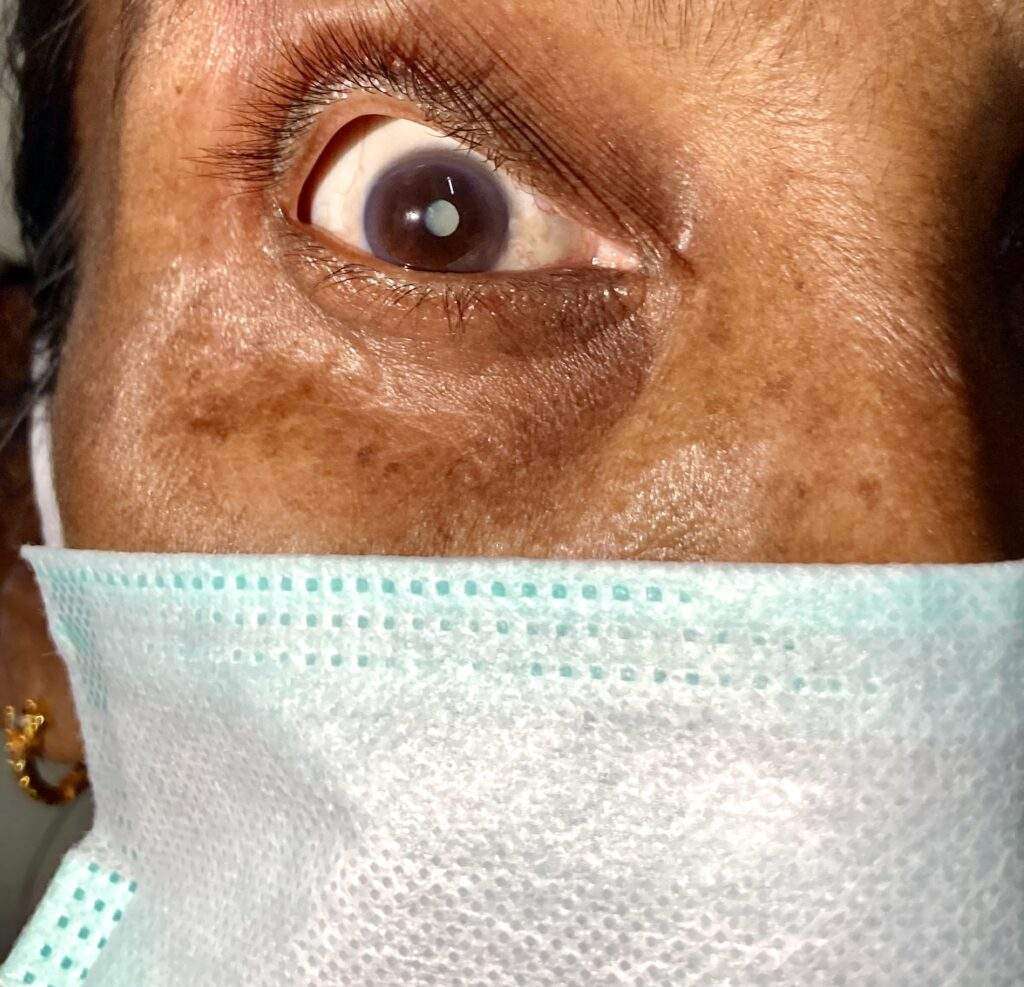
- E stands for Eyes, which refers to visual changes. These visual changes occur suddenly and can include complete vision loss in one eye, double vision, and partial loss of vision in one or both eyes.
- R stands for React, which is a reminder to call nearby health facility immediately if you recognize any of these symptoms. Call even if the symptoms go away and try to remember when they first began..
Identifying and reacting to stroke symptoms quickly is crucial to achieving proper treatment for an individual experiencing a stroke. Recognizing these “FAST” symptoms and getting treatment quickly can minimize damage to the brain and lessen post-stroke complications.
Diagnosis of Stroke
In addition to a physical examination and laboratory tests, physicians may use a variety of advanced imaging diagnostic tests to diagnose a stroke.
In the emergency room, your doctor or stroke emergency team will:
- ask you when the symptoms of the stroke started
- ask you about your medical history
- conduct a physical and neurological examination
- order certain laboratory (blood) tests
- perform imaging tests to help determine what kind of stroke you are having
- request additional tests that might be needed
- request additional tests that might be needed, which could include some of the following:
Imaging Tests
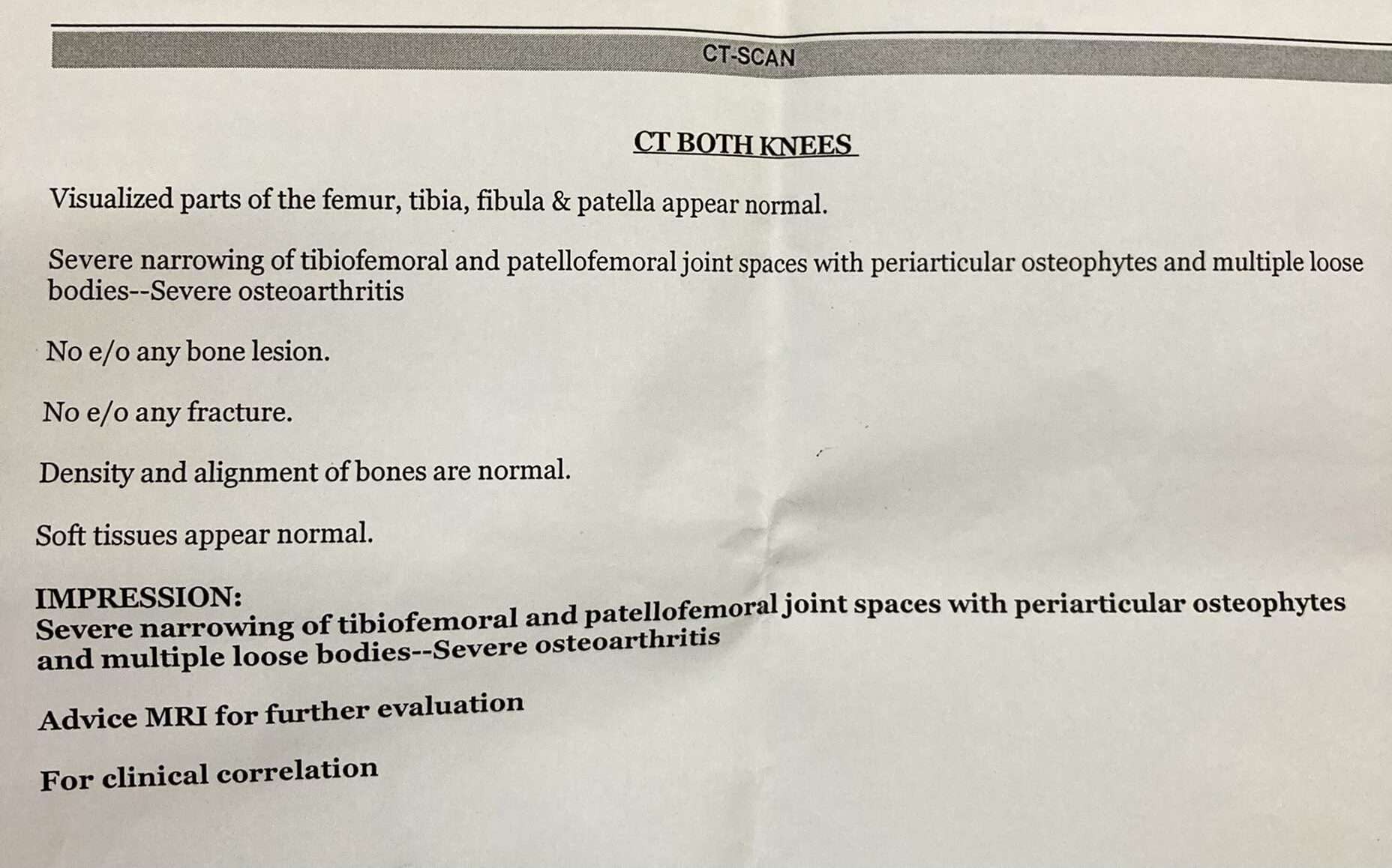
CT scan (computed tomography)
An imaging test of the brain that uses radiation to create a picture (like an X-ray) of the brain. It’s usually one of the first tests given to a patient with stroke symptoms as test results give valuable information about the cause of stroke and the location and extent of brain tissue affected.
MRI (magnetic resonance imaging)
An MRI uses a large magnetic field to produce an image of the brain. Like the CT scan, it shows the location and extent of brain injury. The image produced by MRI is sharp and detailed, so it’s often used to diagnose small, deep injuries and may help determine a possible cause of the stroke.
Echocardiogram
An ultrasound imaging procedure used to assess the heart’s function and structures. It can be used to check for conditions such as heart disease, congenital birth defects, heart failure, pericarditis (an inflammation of the lining of the heart) or disease of the valves which might identify the cause of the stroke.
Blood Flow Tests
Carotid artery ultrasound
A carotid artery ultrasound may be ordered if your doctor hears an abnormal sound over your carotid artery caused by disturbances in the blood flow. This diagnostic test takes images of the blood flowing through the arteries and it can detect how severe the narrowing is from plaque buildup.
Cerebral angiography/cerebral arteriography
A cerebral angiography/cerebral arteriography can be performed to diagnose and show the degree of carotid artery stenosis. This test feeds a catheter from your groin, through your aorta and into the carotid artery. An injectable contrast dye is then inserted into the artery while images of the area are captured. This dye allows your doctor to view the arteries in a more enhanced field of view to detect any vessel abnormality. This test is similar to a catheterization to the heart.
Prevention of Stroke
Many strokes can be prevented in the first place by minimizing risk factors. Maintaining a healthy body weight, staying physically active and controlling blood pressure reduce the risk of stroke. Other stroke prevention steps include stopping smoking, eating a healthy diet and managing blood sugar levels.