Pleural Effusion: Fluid in Pleural Cavity
Pleural Effusion
Pleural effusion, sometimes referred to as “water on the lungs,” is the build-up of excess fluid between the layers of the pleura outside the lungs. The pleura are thin membranes that line the lungs and the inside of the chest cavity and act to lubricate and facilitate breathing. Normally, a small amount of fluid is present in the pleura.
Symptoms
Some patients with pleural effusion have no symptoms, with the condition discovered on a chest X-ray that is performed for another reason. The patient may have unrelated symptoms due to the disease or condition that has caused the effusion. Symptoms of pleural effusion include:
- Chest pain
- Dry, non-productive cough
- Dyspnea (shortness of breath, or difficult, labored breathing)
- Orthopnea (the inability to breathe easily unless the person is sitting up straight or standing erect)
Causes
The most common causes of transudative (watery fluid) pleural effusions include:
- Heart Failure
- Pulmonary Embolism
- Cirrhosis
- Post open heart surgery
Exudative (protein-rich fluid) pleural effusions are most commonly caused by:
- Pneumonia including Tuberculosis
- Cancer
- Pulmonary Embolism
- Kidney Disease
- Inflammatory disease
Other less common causes of pleural effusion include:
- Autoimmune disease
- Bleeding (due to chest trauma)
- Chylothorax (due to trauma)
- Rare chest and abdominal infections
- Asbestosis pleural effusion (due to exposure to asbestos)
- Meig’s syndrome (due to a benign ovarian tumor)
- Ovarian hyperstimulation syndrome
Certain medications, abdominal surgery and radiation therapy may also cause it. It may occur with several types of cancer including lung cancer, breast cancer and lymphoma. In some cases, the fluid itself may be malignant (cancerous), or may be a direct result of chemotherapy.
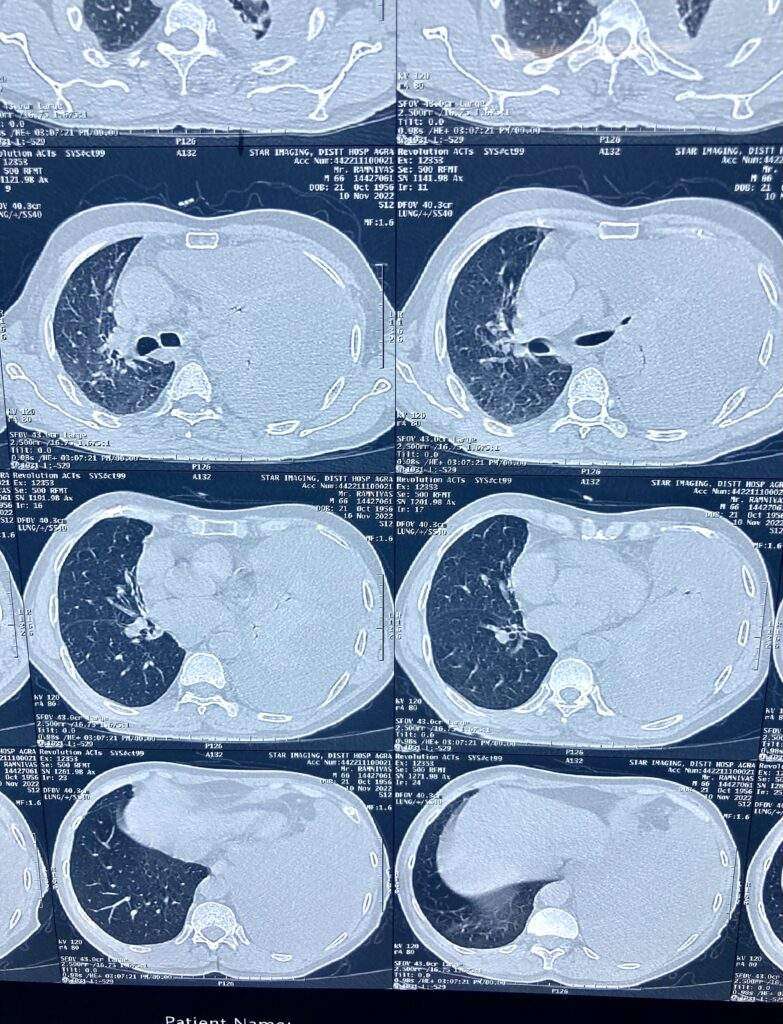
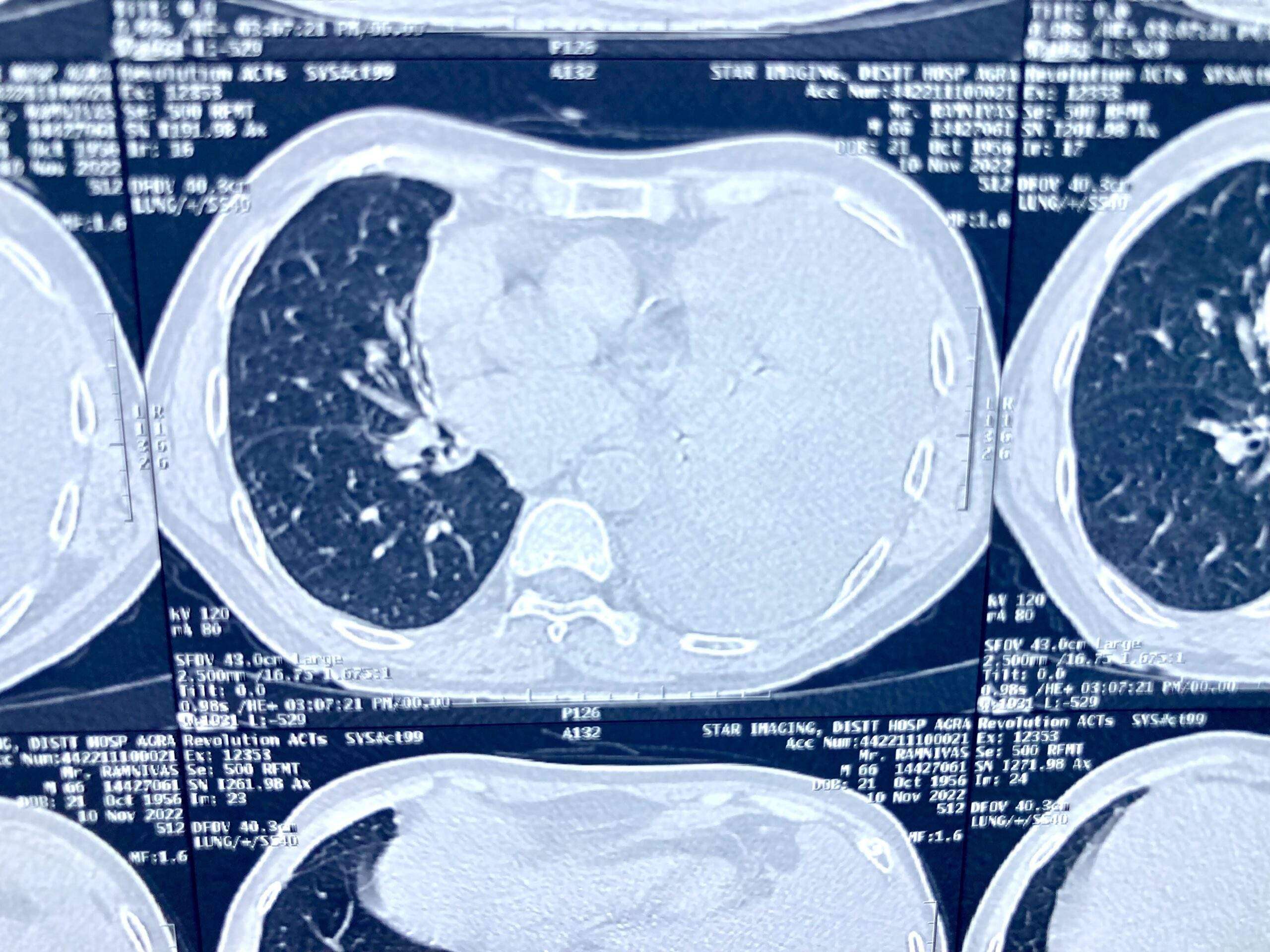
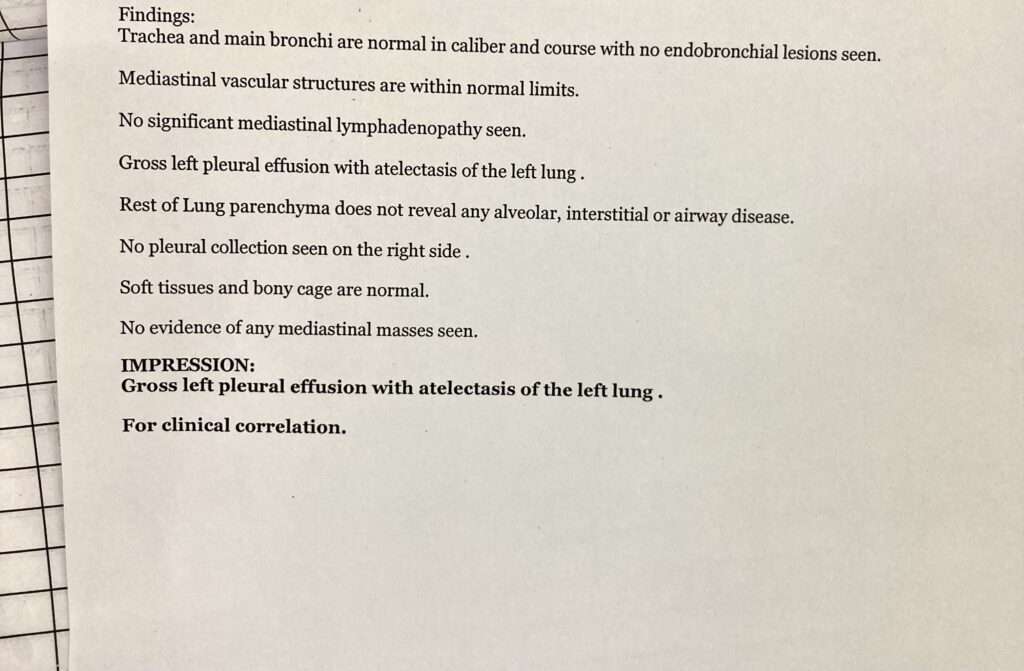
Diagnosis
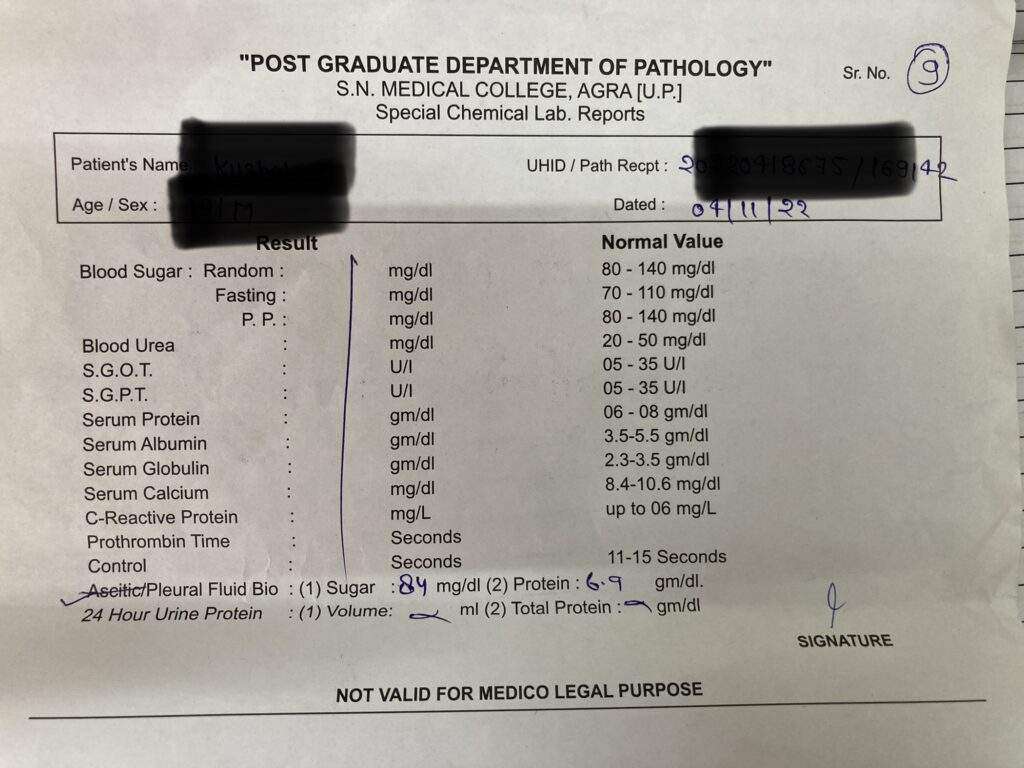
The tests most commonly used to diagnose and evaluate include:
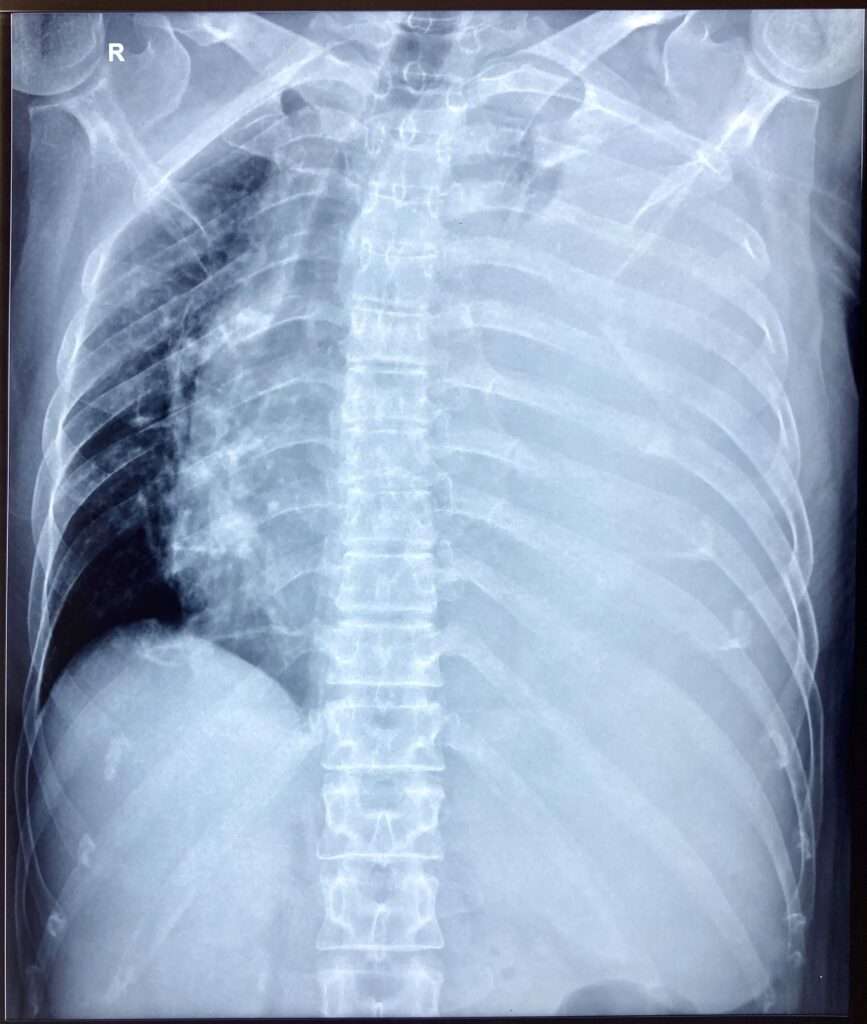
- Chest X-ray
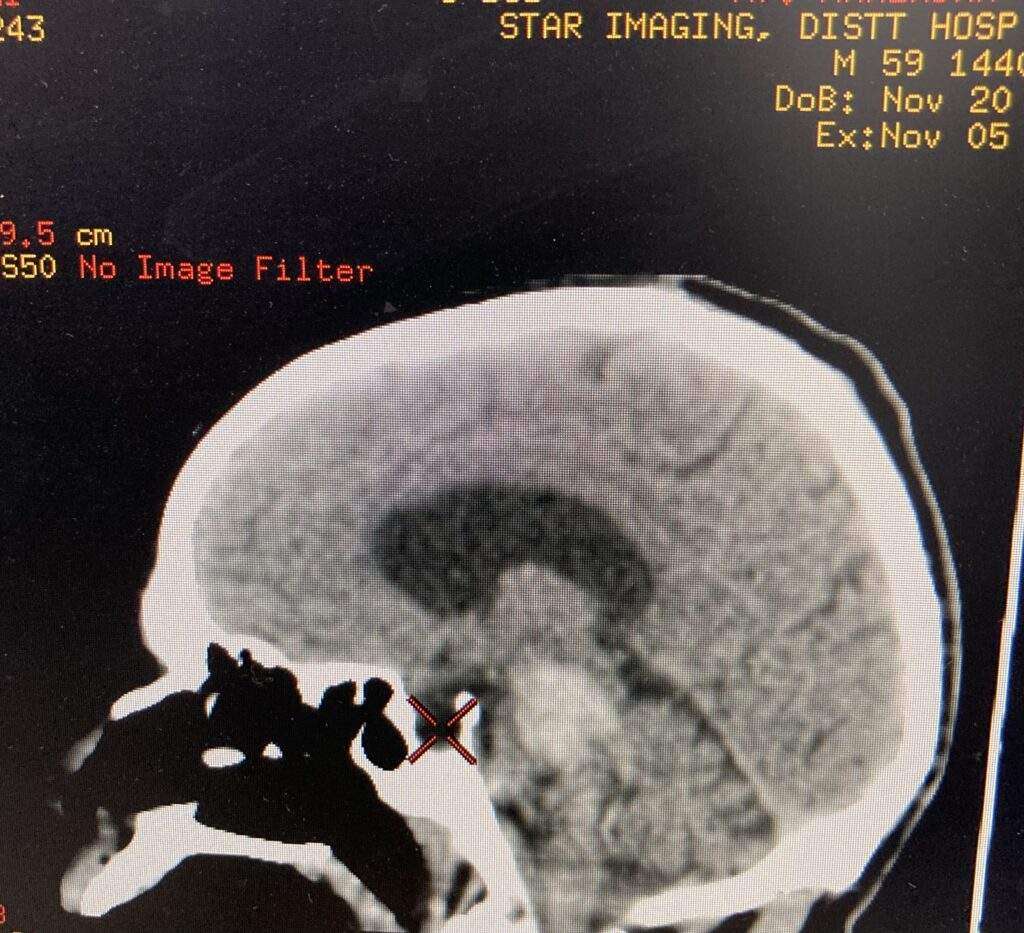
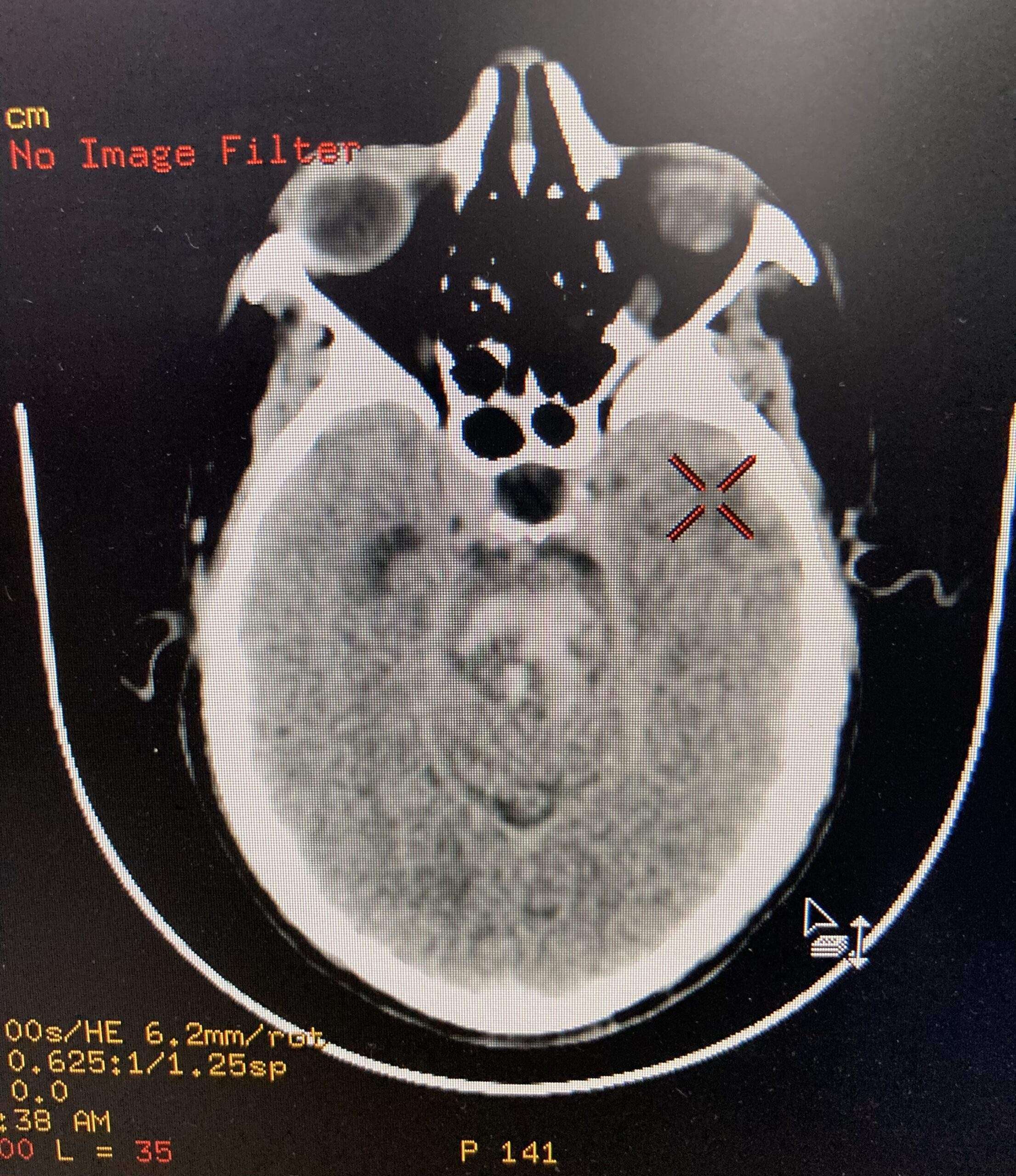
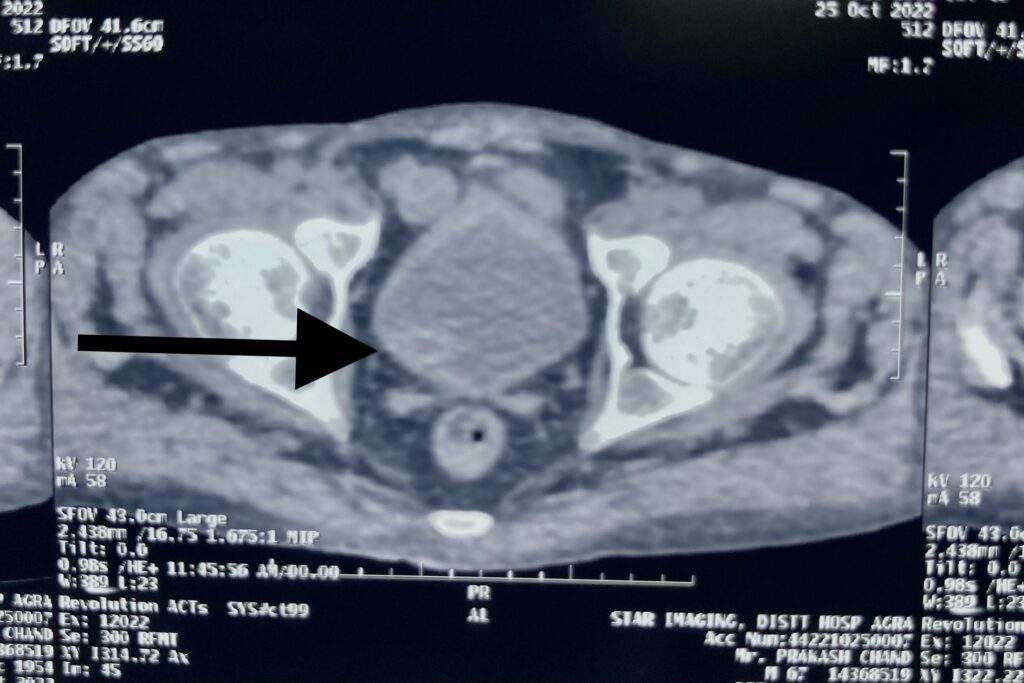
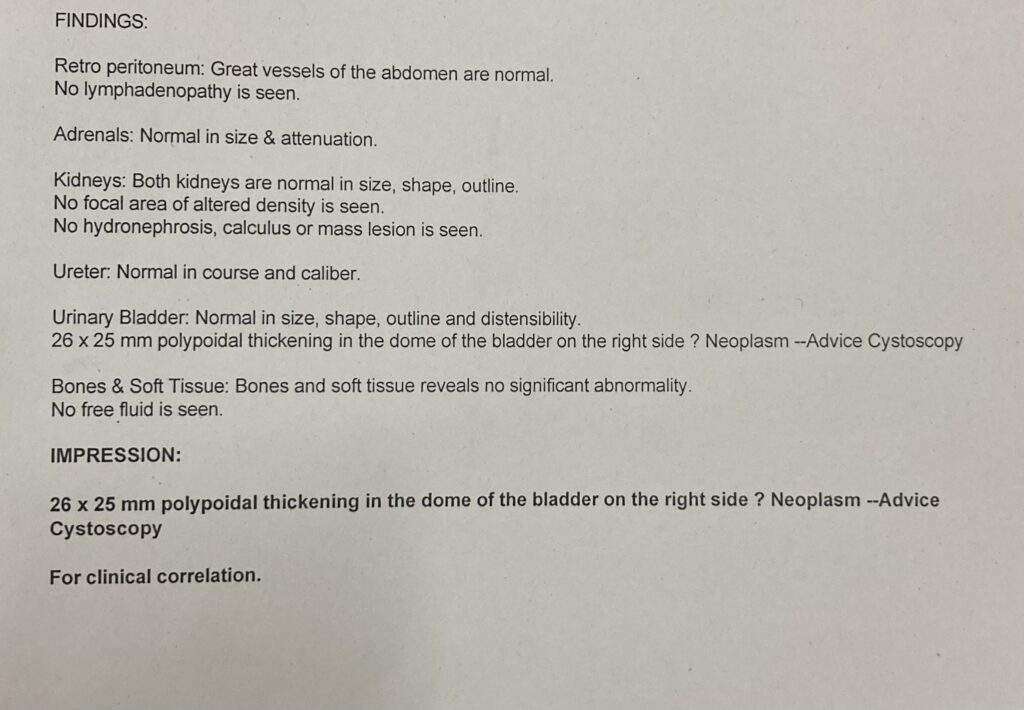
- Computed Tomography (CT) of the chest
- Ultrasonography of the chest
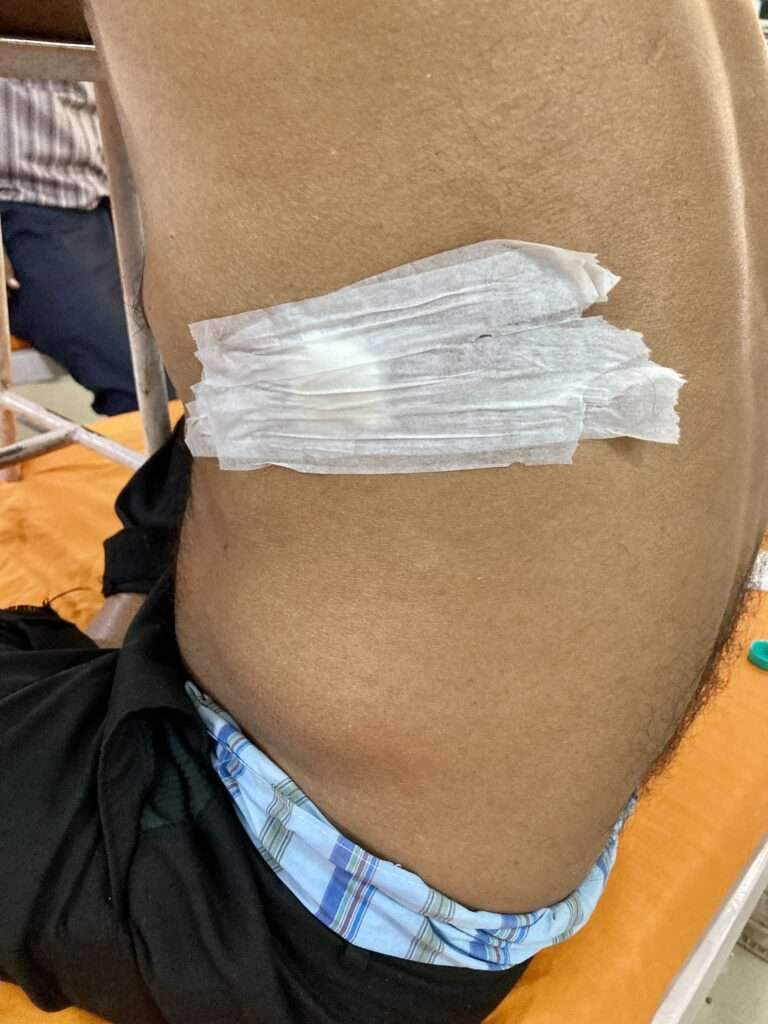
- Thoracentesis (a needle is inserted between the ribs to remove a biopsy, or sample of fluid)
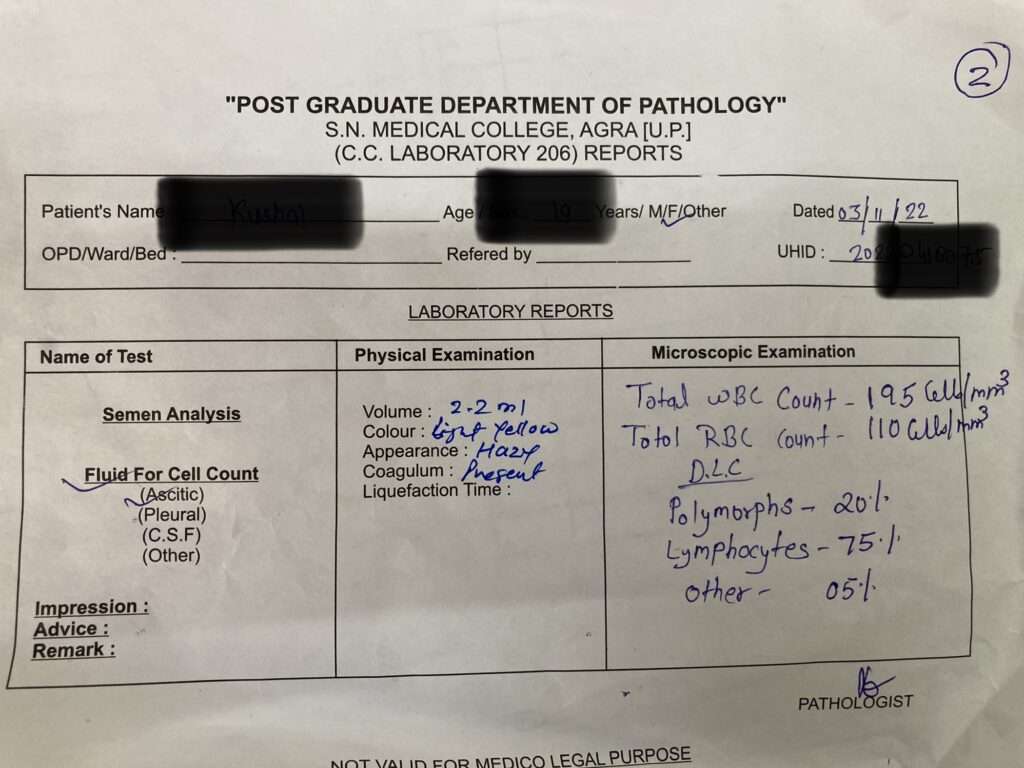
- Pleural fluid analysis (an examination of the fluid removed from the pleura space)


When it has remained undiagnosed despite previous, less-invasive tests, thoracoscopy may be performed. Thoracoscopy is a minimally invasive technique, also known as video-assisted thoracoscopic surgery, or VATS, performed under general anesthesia that allows for a visual evaluation of the pleura). Often, treatment of the effusion is combined with diagnosis in these cases.
Treatment
- Treatment is based on the underlying condition and whether the effusion is causing severe respiratory symptoms, such as shortness of breath or difficulty breathing.
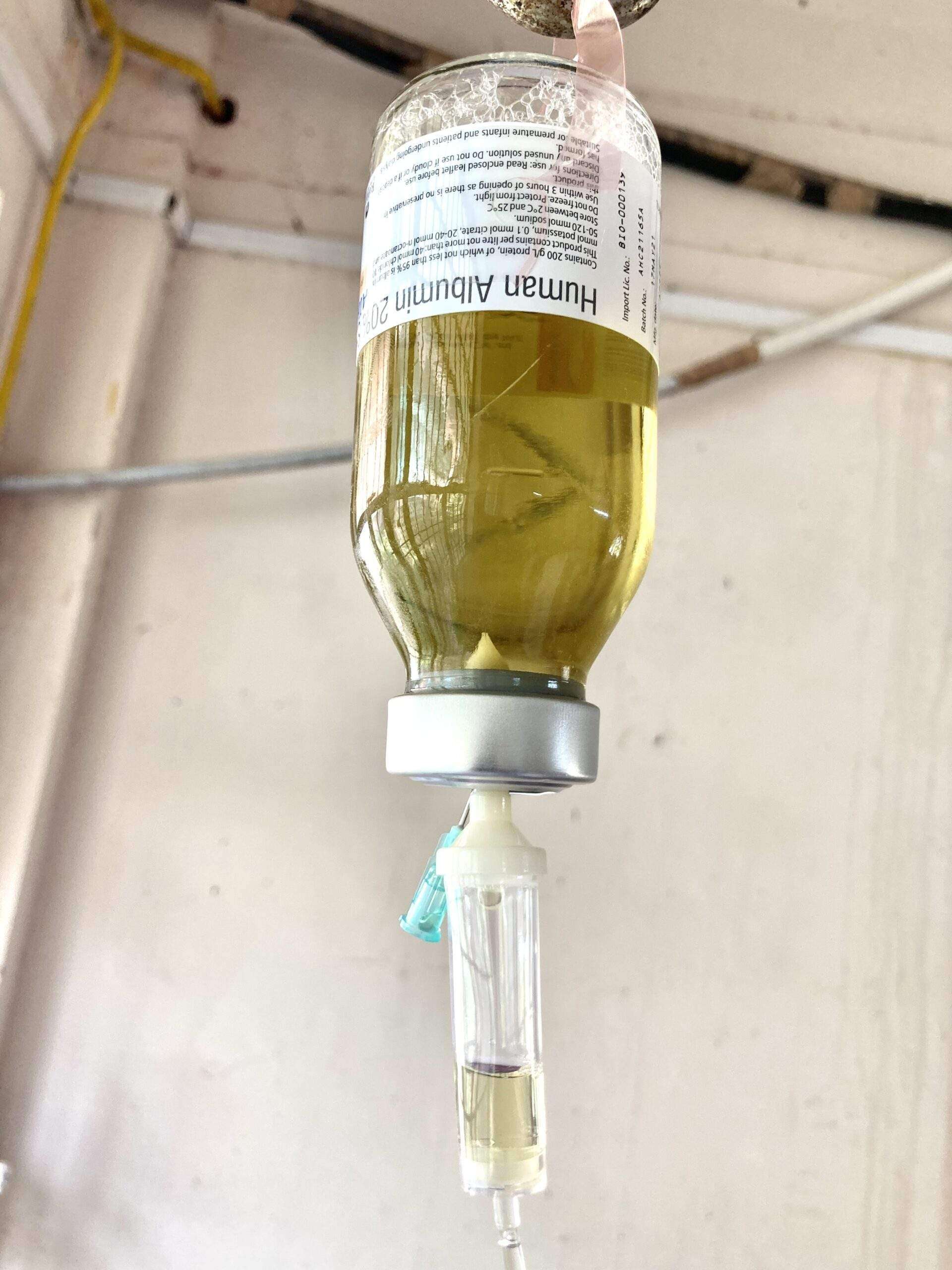
- Diuretics and other heart failure medications are used to treat pleural effusion caused by congestive heart failure or other medical causes. A malignant effusion may also require treatment with chemotherapy, radiation therapy or a medication infusion within the chest.
- A pleural effusion that is causing respiratory symptoms may be drained using therapeutic thoracentesis or through a chest tube (called tube thoracostomy).
- For patients who that are uncontrollable or recur due to a malignancy despite drainage, a sclerosing agent (a type of drug that deliberately induces scarring) occasionally may be instilled into the pleural cavity through a tube thoracostomy to create a fibrosis (excessive fibrous tissue) of the pleura (pleural sclerosis).
- Pleural sclerosis performed with sclerosing agents (such as talc, doxycycline, and tetracycline) is 50 percent successful in preventing the recurrence of pleural effusions.
Surgery
If cannot be managed through drainage or pleural sclerosis may require surgical treatment.
The two types of surgery include:
Video-assisted thoracoscopic surgery (VATS)
A minimally-invasive approach that is completed through 1 to 3 small (approximately ½ -inch) incisions in the chest. Also known as thoracoscopic surgery, this procedure is effective in managing pleural effusions that are difficult to drain or recur due to malignancy. Sterile talc or an antibiotic may be inserted at the time of surgery to prevent the recurrence of fluid build-up.
Thoracotomy (Also referred to as traditional, “open” thoracic surgery)
A thoracotomy is performed through a 6- to 8-inch incision in the chest and is recommended for pleural effusions when infection is present. A thoracotomy is performed to remove all of the fibrous tissue and aids in evacuating the infection from the pleural space. Patients will require chest tubes for 2 days to 2 weeks after surgery to continue draining fluid.
Surgeon will carefully evaluate you to determine the safest treatment option and will discuss the possible risks and benefits of each treatment option.