BREATHE EASY THIS DIWALI 2022
Measures to breathe easy this Diwali?
Breathe easy this Diwali which is arguably India’s biggest festival which is synonymous with lights, lamps, colors and of course, firecrackers. However, this is also the time when air quality deteriorates drastically. The air is chocked with various forms of pollutants with the problem compounded by pollution caused by the increased movement of vehicles.
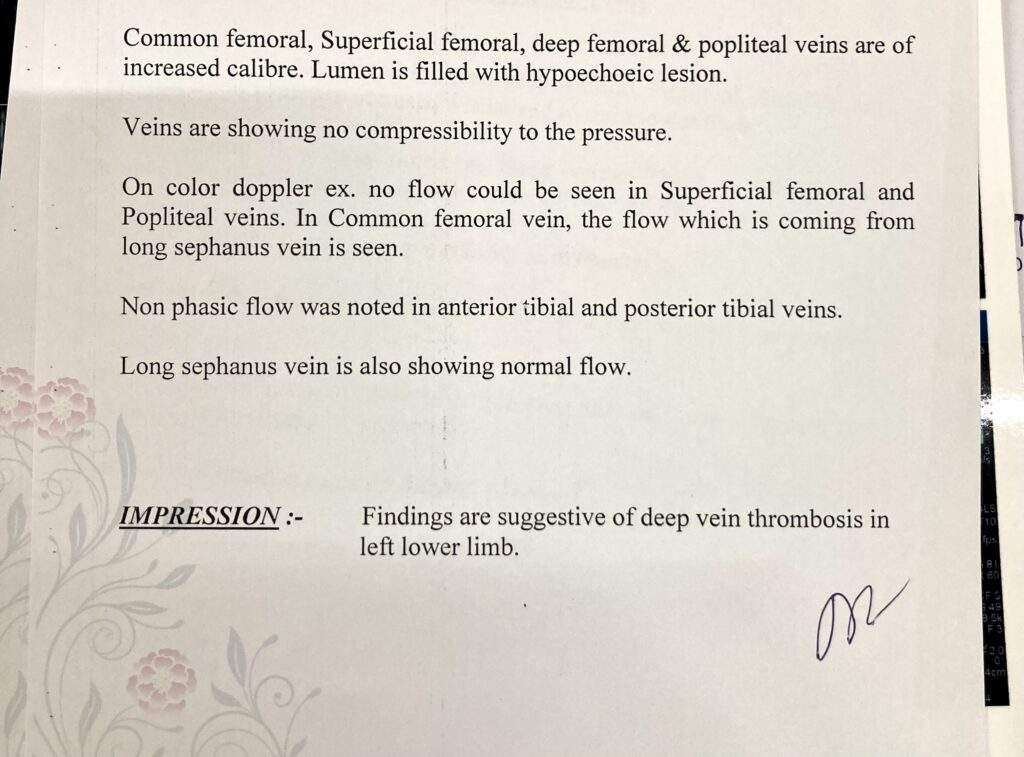
Patients visiting to the hospitals with complaints of severe respiratory disorders during Diwali festival have been increasing for the last five years. These include asthma, ARDS, and exacerbations of chronic lung disorders (COPD), all associated with breathing in polluted and toxic air. The problem of pollution is because of the effects of fireworks in Diwali. It is more severe in cities as the growing number of vehicles adds to the problem.
Air quality takes a deep plunge as the problem gets compounded. Depending on the size of these particles, they cause a variety of illnesses ranging from mild temporary irritation to serious chronic diseases such as cancer.
Particles with a diameter of 10 micrometers (PM 10) and less are considered the most harmful as they are small enough to evade the body’s filters and pass through the entire respiratory system. Travelling from the upper respiratory tract which consists of the nose, pharynx and larynx, the smaller particles end up accumulating in the lower respiratory tract (bronchioles, alveolar ducts, and alveolar sacs) where gas exchanges occur. These are eventually removed by the macrophages of the immune system.
When there is an increased number of particulate matter in the air along with gases, the chances of COPD exacerbations increase. Certain groups of people are particularly susceptible, such as:
Children – Children spend a lot of time playing outdoors and this is the reason why they run a high risk of getting affected by smog. Regular exposure to air pollution (smog) can cause asthma and even other harmful respiratory ailments.
People who do outdoor activities – Anyone who works outdoor is more susceptible to air pollution. Regular exposure and can deteriorate their health causing several respiratory diseases.
People with Asthma & Respiratory disease – People with asthma or chronic respiratory diseases are at a high risk of health hazards caused by smog. They will experience the adverse effects of air pollution much sooner compared to others. Continuous exposure to smog can aggravate lung diseases, heart disease and stroke.
Elderly People – Senior citizens have a weak immune system. Owing to this condition, elderly people are at increased risk of getting affected by air pollution, which can cause cardiac arrhythmias and heart attacks, asthma attacks and many more.
Dry hacking coughs, shortness of breath, chest tightness, wheezing, nasal complaint along with sneezing are some of the common complaints of patients during this time. Air pollution not only affects your lungs but other organs. Thus, it is important to know the health hazards during Diwali time and take precautions accordingly.
- Upper Respiratory Tract Infection: The Post-Diwali period usually witnesses a surge in the number of people with complaints of irritation in the eyes and throat, dry cough and fever. While last year’s smog lingered in the atmosphere, many people who otherwise remain healthy, also experienced irritation in eyes and chest and a general feeling of suffocation.
- Bronchitis: The deadly chemicals used in crackers release fumes and gases that can lead to the inflammation of the bronchial tubes leading to acute attacks.
- Asthma: The condition of asthma patients usually exacerbates during this period because of the toxic fumes in the air.
- COPD: The risk of Chronic Obstructive Pulmonary Disease (COPD) increases during festivals like Diwali when the level of suspended particulate matter becomes high in the air. It is characterized by prolonged cough with excess sputum.
Persons suffering from asthma, bronchitis and other respiratory ailments should start taking precautions several days before the festive season. Also, it is advisable for affected populations to avoid outdoor physical activities and wait until the levels of fine particles decrease. People suffering from Asthma, if it cannot be avoided should use a N95 face mask, which filters out at least 95% of airborne particles.
A normal surgical mask is of no use as pollutants can pass through it. It is important to keep inhalers handy. If one experiences breathlessness then it is advisable to move away from smoggy surroundings and sit in a room with the doors and windows shut and the air-conditioning on. Patients are supposed to continue their treatment for chronic lung disease regularly and consult pulmonologist at regular intervals. It is important to keep an inhaler or nebulizer at hand to dilate your airways. Rush to a hospital if you don’t feel better after inhalation.
Do’s & Don’ts to Stay Safe and breathe easy this Diwali
DOs
- Use Multi Layered Masks: While going out, ensure that your nose and mouth are covered with a good quality mask to ban the entry of harmful particles in your respiratory tract. If you don’t have a mask, simply use a handkerchief or cloth to cover up.
- Use Air Purifiers: Air inside closed spaces is more polluted than outside air. It’s advisable to install air purifiers in at homes and offices that allow only a little movement of air.
- Use Air Purifying Plants: Your home and office must have plenty of plants that purify the air. A noteworthy point here is that there must be a variety of such plants and they must be spaced appropriately.
- Use Air Quality Checking Apps: Before you go out, check the level of pollution through various Apps. If the air quality is severe, avoid going out at all.
- Moisturize Your Nostrils: Moisturizing your nostrils helps in restricting the entry of fine particulate matter through your nose.
DON’Ts
- Morning and Evening Walks/Runs: Air quality is worst in the mornings. Simply avoid morning and evening walks or running outside altogether till air quality improves.
- Heavy Exercising: Do only light exercises, as heavy exercises require heavy breathing.
- Eating Fried/Junk Food: Ensure you eat light, healthy, fiber rich and fat free food to feel healthier and fresh.
- Travelling on two wheelers: Say No to travelling on two wheelers- this can be hazardous for your health.
Human life is above all and good health is a prerequisite of a happy life. We urge everyone to celebrate Diwali responsibly this year- in a way which makes every face glow with a smile and does not put anyone at any kind of health risk.
“Wishing You All, Happy & Safe Diwali”