The Nobel Prize in Physiology or Medicine 2022
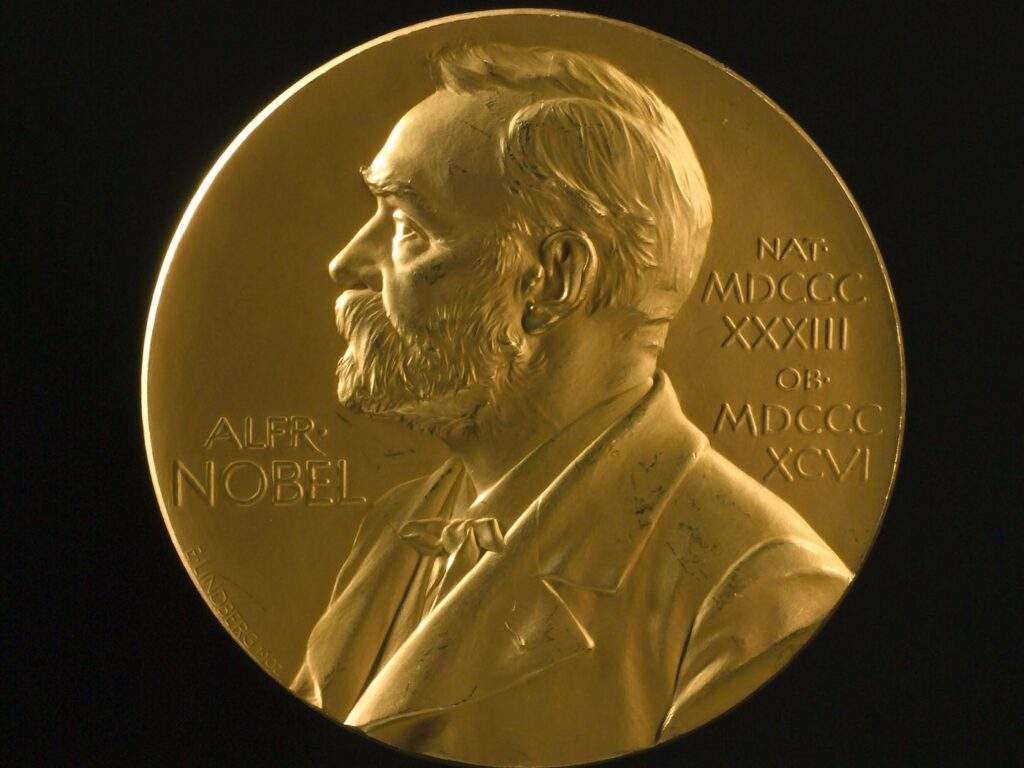
Rule of Odds in spleen: 1” thick, 3” broad, 5” long, 7” ounces weight, underlies 9-11 ribs
A normal, healthy spleen is up to 12 cm long and 70 g in weight. An enlarged spleen may be up to 20 cm long and can weigh more than 1,000 g. Several things can cause your spleen to enlarge, including inflammation, fat storage, pooled blood, benign or malignant growths and overproduction of cells. Some causes are temporary and others may indicate a chronic or progressive condition.
An enlarged spleen typically causes no signs or symptoms, but sometimes it causes:
See your doctor promptly if you have pain in your left upper belly, especially if it’s severe or the pain gets worse when you take a deep breath.
A number of infections and diseases can cause an enlarged spleen. The enlargement might be temporary, depending on treatment. Contributing factors include:
Your spleen is tucked below your rib cage next to your stomach on the left side of your belly. Its size generally relates to your height, weight and sex.
This soft, spongy organ performs several critical jobs, such as:
An enlarged spleen affects each of these jobs. When it’s enlarged, your spleen may not function as usual.
Anyone can develop an enlarged spleen at any age, but certain groups are at higher risk, including:
Potential complications of an enlarged spleen are:
An enlarged spleen is usually detected during a physical exam. Your doctor can often feel it by gently examining your left upper belly. However, in some people — especially those who are slender — a healthy, normal-sized spleen can sometimes be felt during an exam.
Your doctor might order these tests to confirm the diagnosis of an enlarged spleen:
Sometimes more testing is needed to find the cause of an enlarged spleen, including a bone marrow biopsy exam.
A sample of solid bone marrow may be removed in a procedure called a bone marrow biopsy. Or you might have a bone marrow aspiration, which removes the liquid portion of your marrow. Both procedures might be done at the same time.
Liquid and solid bone marrow samples are usually taken from the pelvis. A needle is inserted into the bone through an incision. You’ll receive either a general or a local anesthetic before the test to ease discomfort.
A needle biopsy of the spleen is rare because of the risk of bleeding.
Your doctor might recommend surgery to remove your spleen (splenectomy) for diagnostic purposes when there’s no identifiable cause for the enlargement. More often, the spleen is removed as treatment. After surgery to remove it, the spleen is examined under a microscope to check for possible lymphoma of the spleen.
Treatment for an enlarged spleen focuses on the what’s causing it. For example, if you have a bacterial infection, treatment will include antibiotics.
If you have an enlarged spleen but don’t have symptoms and the cause can’t be found, your doctor might suggest watchful waiting. You see your doctor for reevaluation in 6 to 12 months or sooner if you develop symptoms.
If an enlarged spleen causes serious complications or the cause can’t be identified or treated, surgery to remove your spleen (splenectomy) might be an option. In chronic or critical cases, surgery might offer the best hope for recovery.
Elective spleen removal requires careful consideration. You can live an active life without a spleen, but you’re more likely to get serious or even life-threatening infections after spleen removal.
After spleen removal, certain steps can help reduce your risk of infection, including:
A note from Bhavishya Clinic
An enlarged spleen is a symptom that healthcare providers need to investigate. Whether or not it’s causing you discomfort, it indicates an underlying condition that may need treatment. When it’s temporary, an enlarged spleen won’t harm your overall health. But chronic swelling could damage and endanger your spleen. Your healthcare provider will treat it by treating the underlying cause.
Down syndrome is a disorder caused by a problem with the chromosomes — the pieces of DNA that have the blueprint for the human body. Normally a person has two copies of each chromosome, but a person with Down syndrome has three copies of chromosome 21. The condition also is called trisomy 21.
In a few cases, the extra copy is part of another chromosome (translocation), or found in only some of the person’s cells (mosaicism).
The extra DNA makes the physical and mental characteristics, which include a small head that is flattened in the back; slanted eyes; extra skin folds at the corners of the eyes; small ears, nose and mouth; big-looking tongue; short stature; small hands and feet; and some degree of mental disability.
Down syndrome affects an estimated 1 in 800 births. It’s the most common chromosome problem seen in live births.
In addition to the characteristic physical features and decreased mental abilities, other health problems frequently are seen. These include:
People may develop leukemia more often than those without the disorder, and they are more likely to develop infections, problems with the immune system, skin disorders and seizures.
Infants usually develop more slowly than other children of the same age, although a wide variation is seen. Language development is typically much slower, as is motor development. Their body strength may seem a little weak. For example, most toddlers walk between 12 and 14 months of age, but toddlers walk between 15 and 36 months.
Down syndrome frequently is suspected at birth based on physical appearance. The diagnosis usually is confirmed by a blood test to examine the chromosomes. Additional testing may be done, including chest X-rays, echocardiography and an electrocardiogram, to check for heart problems. Sometimes X-ray studies of the gastrointestinal tract are done as well.
In some cases, Down syndrome is suspected during pregnancy from the results of a fetal ultrasound and blood test that measures the levels of three chemicals (a “triple-screen” test) in a pregnant woman’s blood. If these results are abnormal, further tests can be done to help diagnose it.
Down syndrome continues throughout life.
There is no way to prevent it. However, the chance of having a child with Down syndrome increases as the age of the mother increases.
There is no treatment to reverse the genetic abnormality that causes Down syndrome. However, many of the associated medical and developmental conditions can be treated to:
Many health care professionals may be involved in assessing and planning the course of treatment for a child with Down syndrome. Surgery may be required for cardiac or gastrointestinal problems.
Physical therapy and integrated special education services help children with Down syndrome to make the most of their abilities and reach their potential. Children with Down syndrome usually respond very well to sensory stimulation, exercises to help their muscle control, and activities to help their mental development. School helps children with Down syndrome to learn social, academic and physical skills that may allow them to attain a very high level of functioning and independence.
Most cases of Down syndrome are detected early in life. Call your doctor if you suspect that your child has Down syndrome that has not been diagnosed or if you have questions about your risk of having a child with Down syndrome.
The outlook for a person with Down syndrome varies with the accompanying medical and developmental conditions. The outlook continues to improve, as educators and health care professionals recognize the importance of early interventions to promote both health and development. Advances in medical treatments have greatly improved the life expectancy for people with Down syndrome, with the majority living past age 55.
The overall umbrella theme for the United Nations International Day of Older Persons in 2022 is “Resilience of Older Persons in a Changing World.” This theme will be celebrated by the NGO Committees on Ageing in New York, Geneva and Vienna – each with a unique and complementary approach to the overall theme.
Common conditions in older age include hearing loss, cataracts and refractive errors, back and neck pain and osteoarthritis, chronic obstructive pulmonary disease, diabetes, depression and dementia. As people age, they are more likely to experience several conditions at the same time.
Older age is also characterized by the emergence of several complex health states commonly called geriatric syndromes. They are often the consequence of multiple underlying factors and include frailty, urinary incontinence, falls, delirium and pressure ulcers.




On 14 December 1990, the United Nations General Assembly designated October 1 as the International Day of Older Persons (resolution 45/106). This was preceded by initiatives such as the Vienna International Plan of Action on Ageing, which was adopted by the 1982 World Assembly on Ageing and endorsed later that year by the UN General Assembly.
In 1991, the General Assembly adopted the United Nations Principles for Older Persons resolution 46/91. In 2002, the Second World Assembly on Ageing adopted the Madrid International Plan of Action on Ageing, to respond to the opportunities and challenges of population ageing in the 21st century and to promote the development of a society for all ages.
The composition of the world population has changed dramatically in recent decades. Between 1950 and 2010, life expectancy worldwide rose from 46 to 68 years. Globally, there were 703 million persons aged 65 or over in 2019. The region of Eastern and South-Eastern Asia was home to the largest number of older persons (261 million), followed by Europe and Northern America (over 200 million).
Over the next three decades, the number of older persons worldwide is projected to more than double, reaching more than 1.5 billion persons in 2050. All regions will see an increase in the size of the older population between 2019 and 2050. The largest increase (312 million) is projected to occur in Eastern and South-Eastern Asia, growing from 261 million in 2019 to 573 million in 2050.
The fastest increase in the number of older persons is expected in Northern Africa and Western Asia, rising from 29 million in 2019 to 96 million in 2050 (an increase of 226 per cent). The second fastest increase is projected for sub-Saharan Africa, where the population aged 65 or over could grow from 32 million in 2019 to 101 million in 2050 (218 per cent). By contrast, the increase is expected to be relatively small in Australia and New Zealand (84 per cent) and in Europe and Northern America (48%), regions where the population is already significantly older than in other parts of the world.
Among development groups, less developed countries excluding the least developed countries will be home to more than two-thirds of the world’s older population (1.1 billion) in 2050. Yet the fastest increase is projected to take place in the least developed countries, where the number of persons aged 65 or over could rise from 37 million in 2019 to 120 million in 2050 (225%).
Change the Way You Think About Age!
Patient with severe anemia (HB 1.8 g/dL) only with Leukonychia is treated, responded well on treatment and improved now.
Anemia is a condition in which the blood carries too few red blood cells. Because red blood cells carry oxygen to all tissues of the body, anemia can make it difficult for tissues to get the oxygen they need. This can cause many problems.
There are two main types of anemia:
Common types of anemia include:
Anemia is very common. About 12% of women between the ages of 12 and 49 years have at least mild anemia, mostly from iron deficiency caused by blood loss during menstruation. Up to 20% of pregnant women develop it during their pregnancy.
Mild anemia may not produce any symptoms. It is most often detected through a routine blood test, such as a complete blood cell count.
The condition can cause a variety of symptoms. These include:
Symptoms of anemia vary depending on how low the red blood cell count has dropped.
Treatment depends on the type of anemia an individual has, its cause, and how severe it is. Treatments may be as simple as getting more iron, folic acid, or vitamin B12 in the diet or from supplements to taking medicines and possibly even procedures or surgery to stop blood loss.
1. Start off with confidence and assurance as start determines the end.
2. Be a good listener As Active listening to your patient’s chief complaint and medical problems can sometimes be the ultimate route to the diagnosis.
3. Talking in the patient’s language As Most of the time as medical professionals we are used to using medical terms so often in our practice, that we stick to the same practice and that can leave our patients confused at times.
4. An empathy-driven approach As Just handing the diagnosis to the patient and walking away or giving away the prescription and asking the patient to leave the desk, will not only leave the patient uncertain about the diagnosis and treatment but will also leave a bad taste in the practice and the quality of healthcare.
A good and effective doctor-patient relationship will involve a lot of passive hand-holding by the doctor in order to guide the patient on the right path. And that can be done by using the approach of developing empathy toward the patients. As doctors, it is important that we listen to our patients and understand their points of view even if we have different opinions with respect to them.
5. Communication is not just talking As To develop a good rapport and help the patient understand the treatment and medication condition better the doctors can use the following approaches too to facilitate better communication.
Hand-outs for visual understanding:
Effective communication with patients is an extremely important part of the role of doctors to provide high-quality healthcare. A good doctor-patient relationship can increase job satisfaction and that in turn will help the doctors work and function better. Also, it can be a very big source of motivation and reassurance to the ailing patient. It will mentally help the patient come to terms with the medical condition he or she is suffering and that will in turn help in a better and faster recovery.
It is an unexplained episode of facial muscle weakness or paralysis. It begins suddenly and worsens over 48 hours. This condition results from damage to the facial nerve (the 7th cranial nerve). Pain and discomfort usually occur on one side of the face or head.
It can strike anyone at any age. It occurs most often in pregnant women, and people who have diabetes, influenza, a cold, or another upper respiratory ailment. Bell’s palsy affects men and woman equally. It is less common before age 15 or after age 60.
It is not considered permanent, but in rare cases, it does not disappear. Currently, there is no known cure for Bell’s palsy; however, recovery usually begins 2 weeks to 6 months from the onset of the symptoms. Most people with Bell’s palsy recover full facial strength and expression.
These are the most common symptoms:


These symptoms may look like other conditions or medical problems. Always see your healthcare provider for a diagnosis.

Several things can lead to petechiae, ranging from simple and reversible causes to serious illnesses:
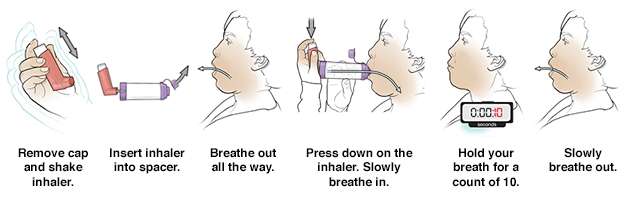
MDI without spacer
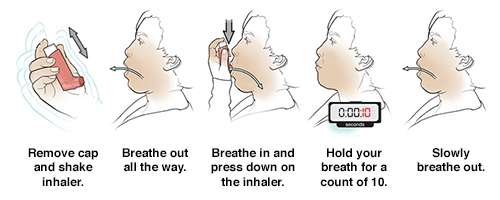
MDI with spacer
On World Lung Day, 25 September 2022, the Forum of International Respiratory Societies (FIRS), of which GOLD is a founding member, calls on governments worldwide to address stark global inequalities in respiratory health.
The COVID-19 pandemic may have subsided, but its impact highlights a global lung health crisis that has not gone away.
Respiratory illnesses affect people in all countries, but disproportionally in low- and middle-income countries (LMICs) where resources for research, prevention, and management are scarce. To address such inequity, we must look beyond medical care to the social and environmental determinants of health such as tobacco use, air pollution, climate change and poverty.
Five respiratory diseases are the commonest causes of illness and death worldwide – chronic obstructive pulmonary disease (COPD), asthma, acute respiratory tract infection or pneumonia, tuberculosis (TB) and lung cancer.