5 Types of Urinary Incontinence

Definition
Urinary incontinence — the loss of bladder control — is a common and often embarrassing problem. The severity ranges from occasionally leaking urine when you cough or sneeze to having an urge to urinate that’s so sudden and strong you don’t get to a toilet in time.
It is not just a medical problem. It can affect emotional, psychological and social life. Many people who have urinary incontinence are afraid to do normal daily activities. They don’t want to be too far away from toilet. It can keep people away from enjoying life.
Though it occurs more often as people get older, urinary incontinence isn’t an inevitable consequence of aging. If urinary incontinence affects your daily activities, don’t hesitate to see your doctor. For most people, simple lifestyle and dietary changes or medical care can treat symptoms of urinary incontinence.
Our urinary system is made up of the kidneys, ureters, bladder and urethra. These parts do several functions. They filter, store and remove waste from your body. Kidneys are the filters of your body. Waste products are removed from your blood by the kidneys, creating urine. The urine then moves down through two thin tubes called the ureters. The ureters connect to the bladder, where the urine will collect until it’s time to leave the body.
Urinary bladder is like a storage tank — once the bladder is full, the brain sends a signal that it’s time to urinate. Urine then leaves the bladder when a muscle opens up (sphincter), allowing the urine to flow freely out of the body through the urethra.
When this system is working smoothly, we usually have time to get to a bathroom before needing to urinate and we don’t experience any leakage of urine. Urinary incontinence can happen when these parts don’t operate as they should. This can happen for many different reasons throughout your life.
Many people think that incontinence is a normal part of aging that can’t be helped. While it is true that your risk of incontinence increases as we get older, there are also treatments available to help you manage this condition. Incontinence doesn’t have to disrupt your life and keep you from being active.
Symptoms
Many people experience occasional, minor leaks of urine. Others may lose small to moderate amounts of urine more frequently.
5 Types of urinary incontinence include:
- Stress incontinence. Urine leaks when you exert pressure on your bladder by coughing, sneezing, laughing, exercising or lifting something heavy.
- Urge incontinence. You have a sudden, intense urge (feel) to urinate followed by an involuntary loss of urine. You may need to urinate often, including throughout the night. Urge incontinence may be caused by a minor condition, such as infection, or a more severe condition such as a neurological disorder or diabetes.
- Overflow incontinence. You experience frequent or constant dribbling of urine due to a bladder that doesn’t empty completely.
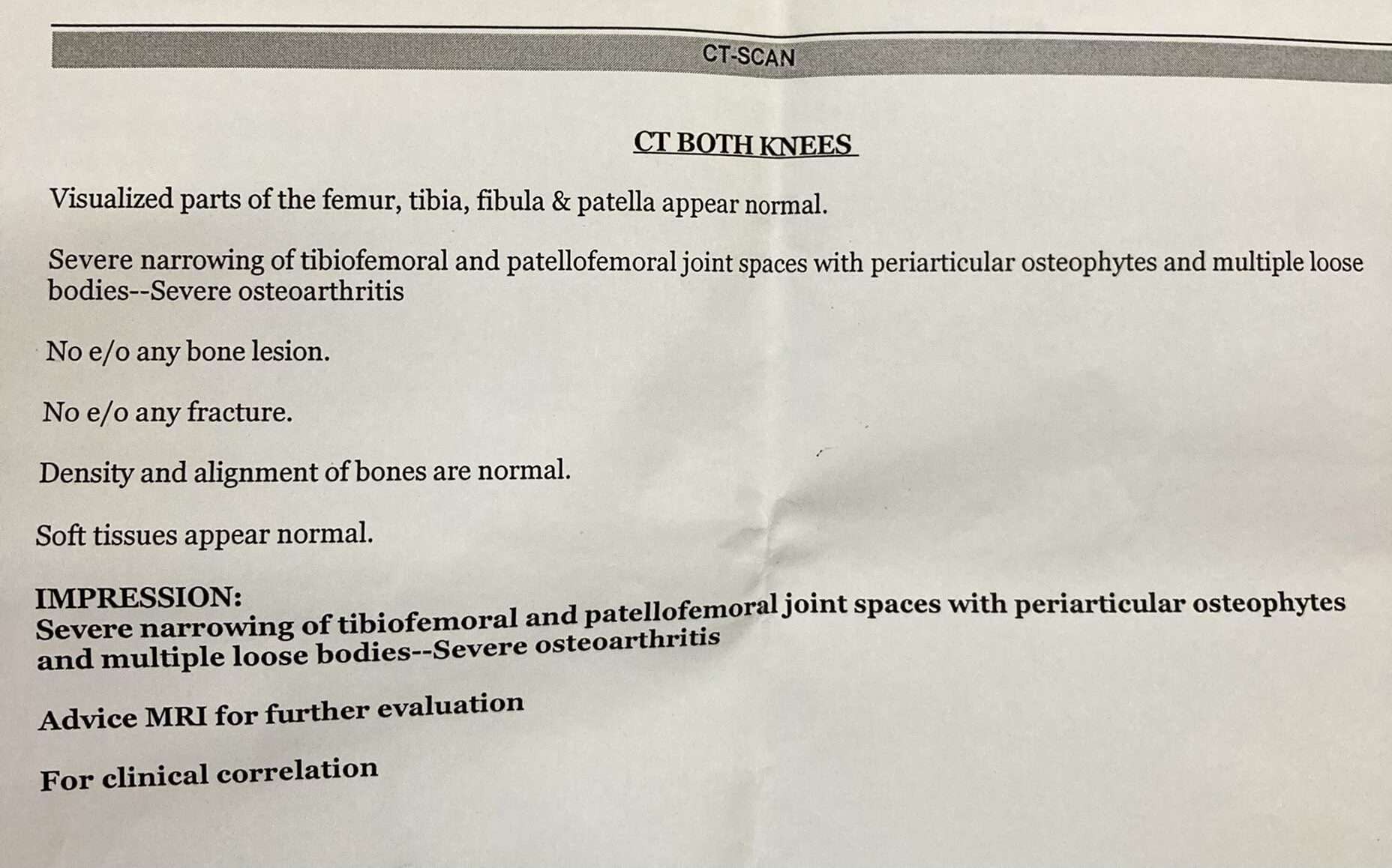
- Functional incontinence. A physical or mental impairment keeps you from making it to the toilet in time. For example, if you have severe arthritis, you may not be able to unbutton your pants quickly enough.
- Mixed incontinence. You experience more than one type of urinary incontinence — most often this refers to a combination of stress incontinence and urge incontinence.
Causes
Urinary incontinence can be caused by everyday habits, underlying medical conditions or physical problems. A thorough evaluation by your doctor can help determine what’s behind your incontinence.
Temporary urinary incontinence
Certain drinks, foods and medications may act as diuretics — stimulating your bladder and increasing your volume of urine. They include:
- Alcohol
- Caffeine
- Carbonated drinks and sparkling water
- Artificial sweeteners
- Chocolate
- Chili peppers
- Foods that are high in spice, sugar or acid, especially citrus fruits
- Heart and blood pressure medications, sedatives, and muscle relaxants
- Large doses of vitamin C
Urinary incontinence may also be caused by an easily treatable medical condition, such as:
- Urinary tract infection. Infections can irritate your bladder, causing you to have strong urges to urinate and, sometimes, incontinence.
- Constipation. The rectum is located near the bladder and shares many of the same nerves. Hard, compacted stool in your rectum causes these nerves to be overactive and increase urinary frequency.
Persistent urinary incontinence
Urinary incontinence can also be a persistent condition caused by underlying physical problems or changes, including:
- Pregnancy. Hormonal changes and the increased weight of the fetus can lead to stress incontinence.
- Childbirth. Vaginal delivery can weaken muscles needed for bladder control and damage bladder nerves and supportive tissue, leading to a dropped (prolapsed) pelvic floor. With prolapse, the bladder, uterus, rectum or small intestine can get pushed down from the usual position and protrude into the vagina. Such protrusions may be associated with incontinence.
- Changes with age. Aging of the bladder muscle can decrease the bladder’s capacity to store urine. Also, involuntary bladder contractions become more frequent as you get older.
- Menopause. After menopause, women produce less estrogen, a hormone that helps keep the lining of the bladder and urethra healthy. Deterioration of these tissues can aggravate incontinence.
- Enlarged prostate. Especially in older men, incontinence often stems from enlargement of the prostate gland, a condition known as benign prostatic hyperplasia.
- Prostate cancer. In men, stress incontinence or urge incontinence can be associated with untreated prostate cancer. But more often, incontinence is a side effect of treatments for prostate cancer.
- Obstruction. A tumor anywhere along your urinary tract can block the normal flow of urine, leading to overflow incontinence. Urinary stones — hard, stone like masses that form in the bladder — sometimes cause urine leakage.
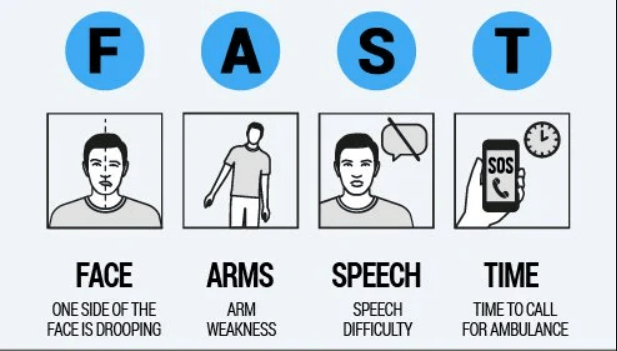
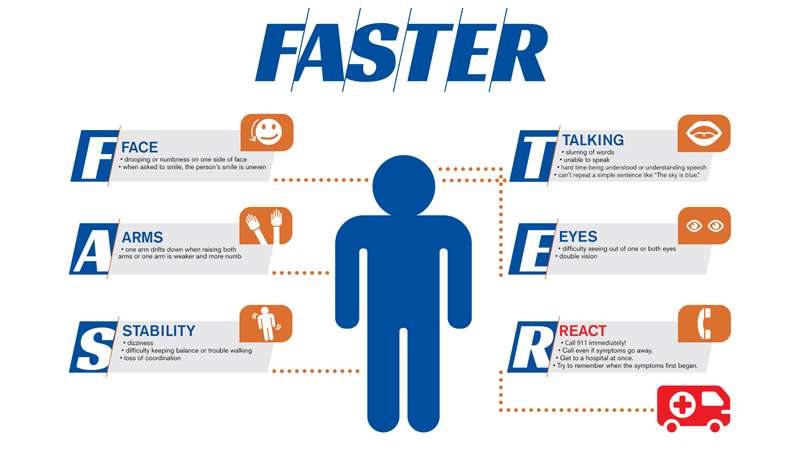
- Neurological disorders. Multiple sclerosis, Parkinson’s disease, a stroke, a brain tumor or a spinal injury can interfere with nerve signals involved in bladder control, causing urinary incontinence.
Risk Factors
Factors that increase your risk of developing urinary incontinence include:
- Gender. Women are more likely to have stress incontinence. Pregnancy, childbirth, menopause and normal female anatomy account for this difference. However, men who have prostate gland problems are at increased risk of urge and overflow incontinence.
- Age. As you get older, the muscles in your bladder and urethra lose some of their strength. Changes with age reduce how much your bladder can hold and increase the chances of involuntary urine release.
- Being overweight. Extra weight increases pressure on your bladder and surrounding muscles, which weakens them and allows urine to leak out when you cough or sneeze.
- Smoking. Tobacco use may increase your risk of urinary incontinence.
- Family history. If a close family member has urinary incontinence, especially urge incontinence, your risk of developing the condition is higher.
- Some diseases. Neurological disease or diabetes may increase your risk of incontinence.
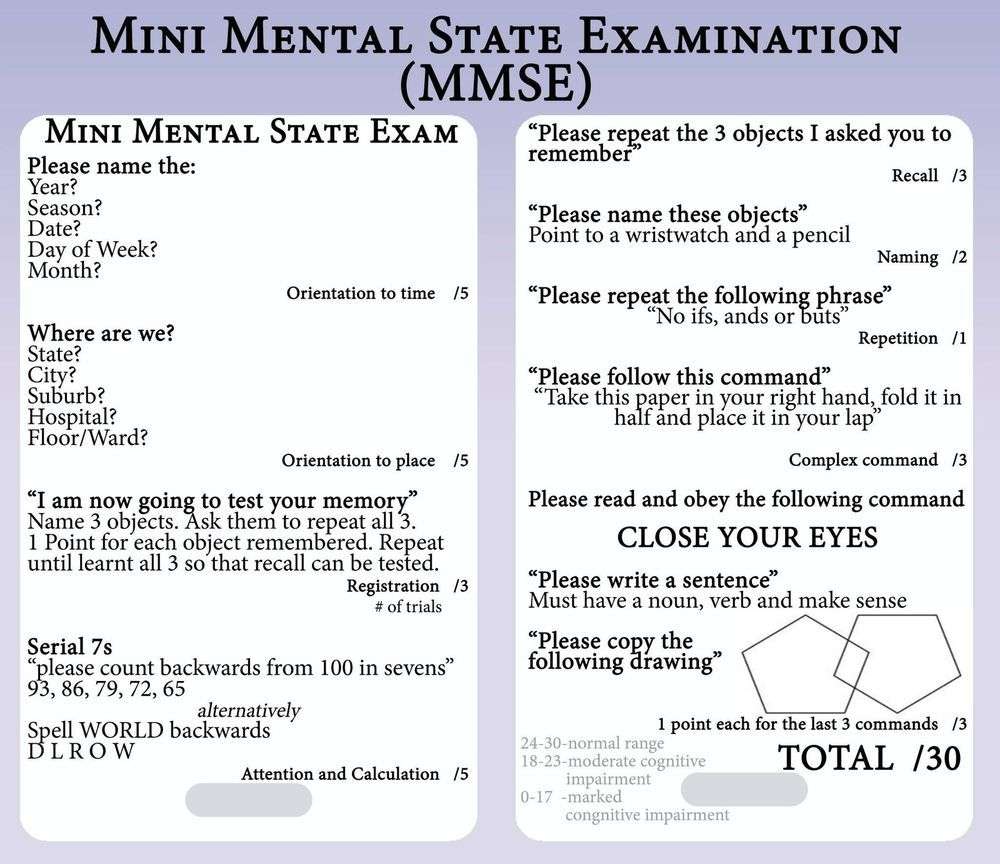
Diagnosis
Your doctor is likely to start with a thorough history and physical exam. You may then be asked to do a simple maneuver that can demonstrate incontinence, such as coughing.
- Urinalysis. A sample of your urine is checked for signs of infection, traces of blood or other abnormalities.
- Bladder diary. For several days you record how much you drink, when you urinate, the amount of urine you produce, whether you had an urge to urinate and the number of incontinence episodes.
- Postvoid residual measurement. You’re asked to urinate (void) into a container that measures urine output. Then your doctor checks the amount of leftover urine in your bladder using a catheter or ultrasound test. A large amount of leftover urine in your bladder may mean that you have an obstruction in your urinary tract or a problem with your bladder nerves or muscles.
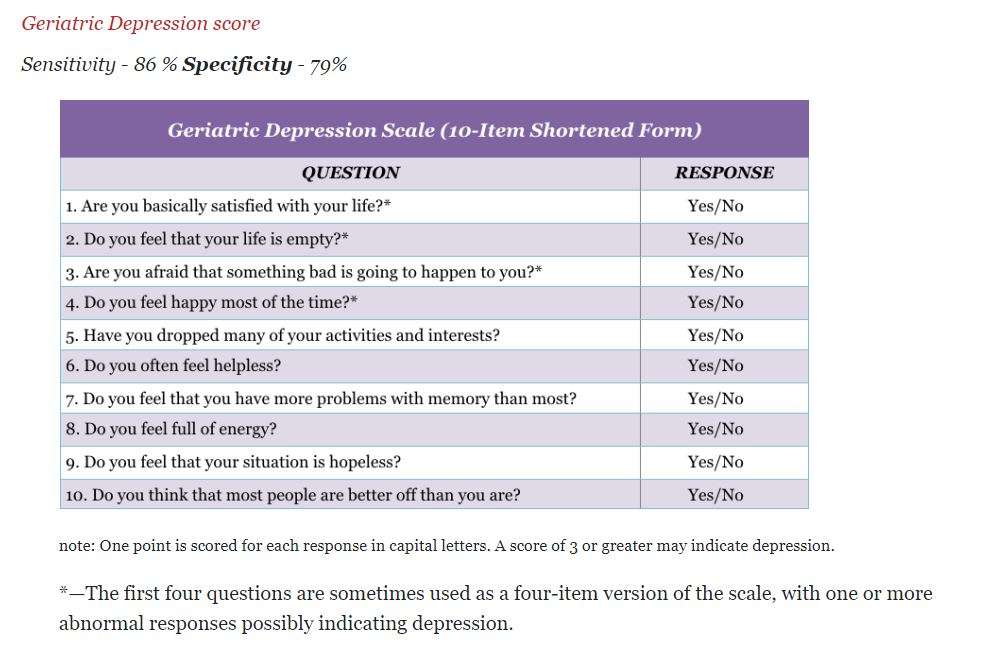
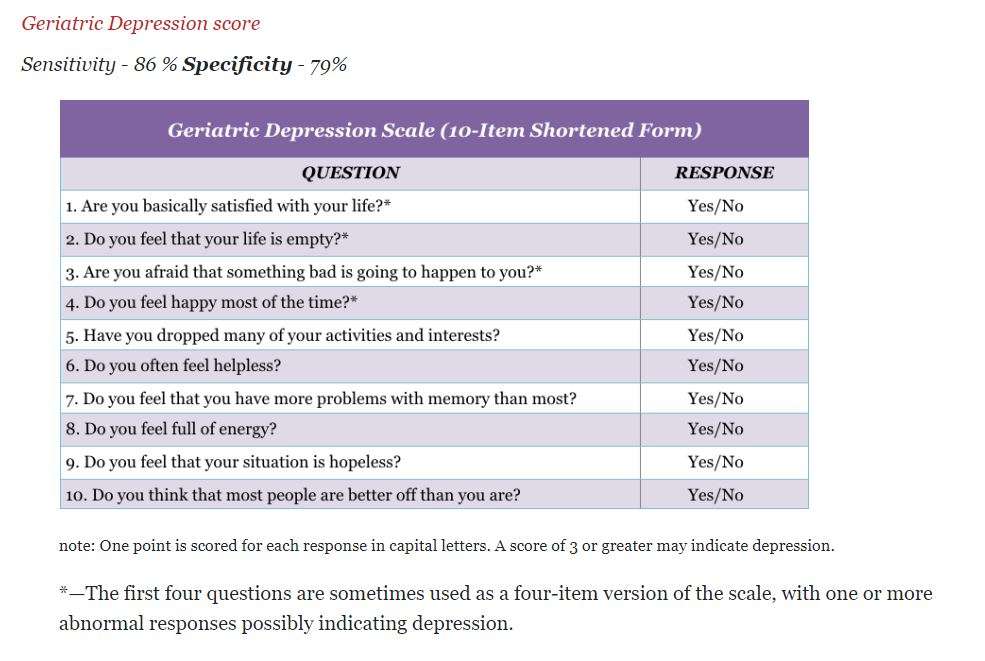
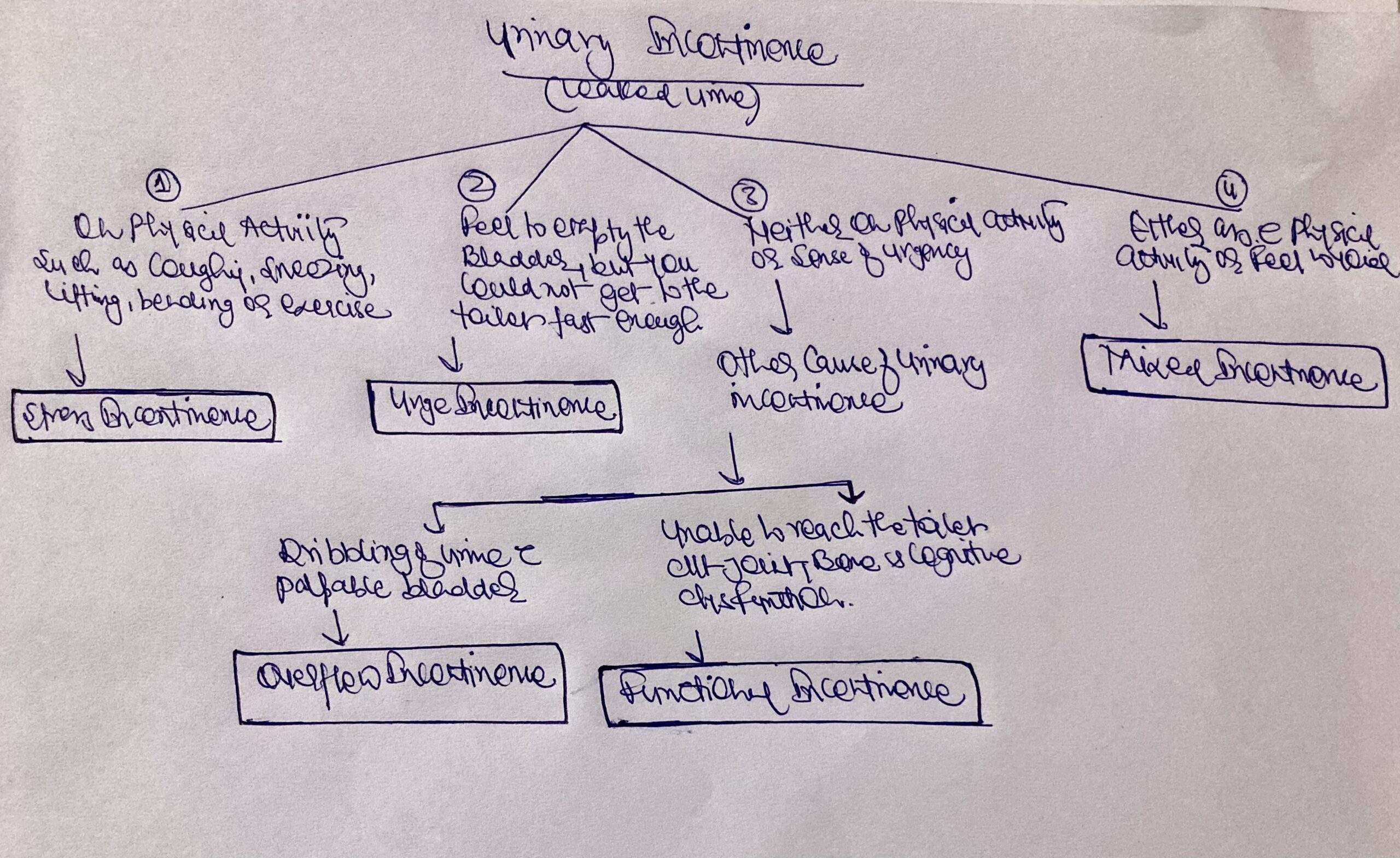
3IQ (Incontinence Questionnaire)
These questions are differentiate between these types of incontinence.
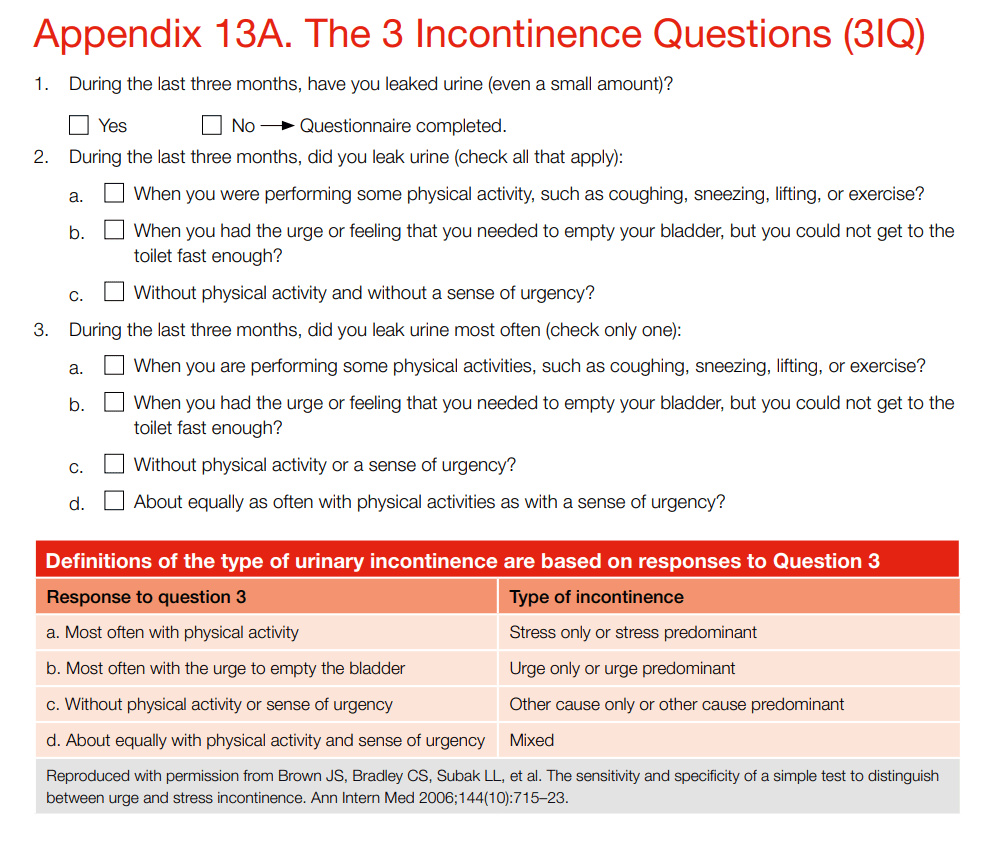
Urinary Incontinence Algorithm
Treatment
Behavioral techniques
- Bladder training, to delay urination after you get the urge to go. You may start by trying to hold off for 10 minutes every time you feel an urge to urinate. The goal is to lengthen the time between trips to the toilet until you’re urinating only every 2.5 to 3.5 hours.
- Double voiding, to help you learn to empty your bladder more completely to avoid overflow incontinence. Double voiding means urinating, then waiting a few minutes and trying again.
- Scheduled toilet trips, to urinate every two to four hours rather than waiting for the need to go.
- Fluid and diet management, to regain control of your bladder. You may need to cut back on or avoid alcohol, caffeine or acidic foods. Reducing liquid consumption, losing weight or increasing physical activity also can ease the problem.
Pelvic Floor Muscles Exercises
Also known as Kegel exercises, these techniques are especially effective for stress incontinence but may also help urge incontinence.
To do pelvic floor muscle exercises, imagine that you’re trying to stop your urine flow. Then:
- Tighten (contract) the muscles you would use to stop urinating and hold for five seconds, and then relax for five seconds. (If this is too difficult, start by holding for two seconds and relaxing for three seconds.)
- Work up to holding the contractions for 10 seconds at a time.
- Aim for at least three sets of 10 repetitions each day.
To help you identify and contract the right muscles, your doctor may suggest that you work with a pelvic floor physical therapist or try biofeedback techniques
Medications
Medications commonly used to treat incontinence include:
- Anticholinergics. These medications can calm an overactive bladder and may be helpful for urge incontinence. Examples include oxybutynin, tolterodine, darifenacin, solifenacin.
- Mirabegron. Used to treat urge incontinence, this medication relaxes the bladder muscle and can increase the amount of urine your bladder can hold. It may also increase the amount you are able to urinate at one time, helping to empty your bladder more completely.
- Alpha blockers. In men who have urge incontinence or overflow incontinence, these medications relax bladder neck muscles and muscle fibers in the prostate and make it easier to empty the bladder. Examples include tamsulosin, alfuzosin, silodosin.
- Topical estrogen. Applying low-dose, topical estrogen in the form of a vaginal cream, ring or patch may help tone and rejuvenate tissues in the urethra and vaginal areas.
Absorbent pads and Catheters
- Pads and protective garments. Most products are no more bulky than normal underwear and can be easily worn under everyday clothing. Men who have problems with dribbles of urine can use a drip collector — a small pocket of absorbent padding that’s worn over the penis and held in place by close-fitting underwear.
- Catheter. If you’re incontinent because your bladder doesn’t empty properly, doctor may recommend that you learn to insert a soft tube (catheter) into your urethra several times a day to drain your bladder. You’ll be instructed on how to clean these catheters for safe reuse.
Lifestyle and home remedies
- Use a washcloth to clean yourself.
- Allow your skin to air-dry.
- Avoid frequent washing and douching because these can overwhelm your body’s natural defenses against bladder infections.
- Consider using a barrier cream, such as petroleum jelly or cocoa butter, to protect your skin from urine.
- Ask your doctor about special cleansers made to remove urine that may be less drying than other products.
If you have urge incontinence or nighttime incontinence, make the toilet more convenient:
- Move any rugs or furniture you might trip over or collide with on the way to the toilet.
- Use a night light to illuminate your path and reduce your risk of falling.
If you have functional incontinence, you might:
- Keep a bedside commode in your bedroom.
- Install an elevated toilet seat.
- Widen an existing bathroom doorway.
Complications
- Skin problems. Rashes, skin infections and sores can develop from constantly wet skin.
- Urinary tract infections. Incontinence increases your risk of repeated urinary tract infections.
- Impacts on your personal life. Urinary incontinence can affect your social, work and personal relationships.
Prevention
Urinary incontinence isn’t always preventable. However, to help decrease your risk:
- Maintain a healthy weight
- Practice pelvic floor exercises
- Avoid bladder irritants, such as caffeine, alcohol and acidic foods
- Eat more fiber, which can prevent constipation, a cause of urinary incontinence
- Don’t smoke, or seek help to quit if you’re a smoker
A note from Bhavishya Clinic+
It can be embarrassing to talk about bathroom habits with healthcare provider. This embarrassment shouldn’t stop you from treating incontinence, though. Often, your healthcare provider can help figure out the cause of your bladder control issue and help make it better. You don’t need to deal with it alone. Talk to your healthcare provider about the best ways to treat incontinence so that you can lead a full and active life without worrying about leakage.